This is an automatically translated article.
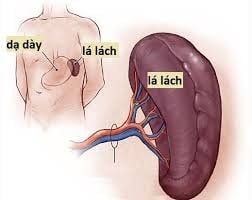
Injury to the spleen is an emergency that needs to be treated early, otherwise splenectomy will be required. However, the symptoms of splenic injury are often confused with many other diseases, leading to delay in emergency care. The following article will inform readers of the knowledge of trauma as well as suture of the spleen.
1. What is a spleen injury?
Injury to the spleen occurs when the abdominal cavity is contusion. Patients will appear some typical symptoms such as abdominal pain, shoulder pain, peritoneal tenderness.
Causes of this injury such as:
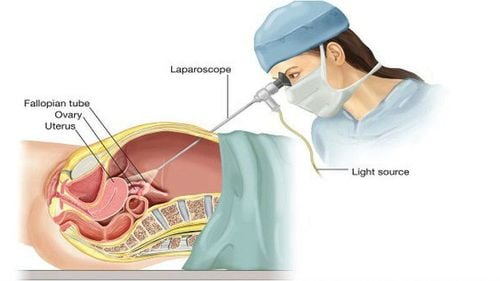
Abdominal cavity is subjected to strong trauma resulting in spleen damage due to car collisions, accidents or being stabbed by sharp objects, bullets... Due to virus causing spleen rupture, specifically EBV virus (infectious mononucleosis or Epstein-Barr virus after organ transplantation – pseudo-lymphoma). Subcapsular hematomas lead to deep lacerations into tissues and cause pedicle rupture. Abdominal gas or white gas appears to cause abdominal injury To determine this injury, the doctor will order to perform a number of tests such as: Exploration of the abdomen by open surgery or laparoscopic surgery, Abdominal CT scan,...
2. Indications and contraindications
According to experts, in cases, the spleen injury does not go deep into the splenic stalk or the superficial wound is less than 3cm can be sutured conservatively.
However, if the patient presents with intestinal perforation and peritonitis requiring bowel resection, suturing the spleen is contraindicated. In addition, patients with hemodynamic abnormalities will not be indicated for this method.
3. The process of suturing the spleen wound
3.1. Preparation On the side of the patient: The patient and his family will be discussed by the doctor about the condition, the process of suturing the spleen as well as the possible risks. At the same time, the patient was resuscitated to ensure hemodynamic stability and prepared for prophylactic antibiotics.
On the hospital side To prepare for the surgery, it is necessary to have a gastroenterologist, a surgeon, a nurse, and a staff member. Necessary medical equipment and instruments such as: Major open surgery kit. – Suture kit – Sewing thread: prolen or premilen 3/0.

Khâu vết thương lách cần chuẩn bị dụng cụ y tế cần thiết
3.2. Procedure The patient is instructed to lie on his or her back. Depending on the surgical requirements, the doctor will place the patient in a high or low position, leaning left or right. Insert the patient's urinary catheter and a dorsal pad across the lower border of the scapula to expose the spleen.
Below is the procedure for suturing the splenic wound:
Step 1: Undergo general anesthesia and intubate the patient. There is a monitor to monitor blood CO2 pressure (PaCO2) and exhaled CO2 pressure (PET CO2).
Step 2: Open the abdomen to the middle white line above the navel, extending down to the patient's navel. Insert gauze into the spleen while continuing to examine the entire abdomen. Assess the extent of damage to the abdominal organs.
Step 3: If there is damage to the spleen, perform the following steps:
To expose the spleen area, or cut the splenic colonic ligament, the doctor will perform splenic flexure. cut the spleen and kidney ligament and the connection between the spleen and the kidney close to the superior pole and the short gastric branches Suture the spleen by steps to bring the spleen out near the incision, suture the spleen with U-shaped stitches along the two edges of the line broken. Pressure sutures can be performed with the greater omentum or oral pledget teflon. Rinse the abdomen and place 1 or 2 drains in the splenic fossa. Close the abdominal incision and end the surgery
4. Monitor and manage complications after suturing spleen wounds
4.1. Follow-up After surgery, the patient was transferred to the recovery room and monitored for postoperative complications within the first 2 days. Administer analgesia and parenteral nutrition until digestion can be restored. 4.2. Management of complications: In case the patient has some complications after surgery such as: bleeding after surgery, hemodynamic instability... In case hemodynamic instability will be further evaluated and indicated for re-operation. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.