This is an automatically translated article.
In Vietnam, patients with gastrointestinal bleeding are increasing. The main cause is varicose veins. What is gastric aneurysm? And if not treated in time, the disease can cause "Death". The following article helps you understand the indications for gastric aneurysm ligation in the management of gastrointestinal bleeding.
1. What is gastric aneurysm?
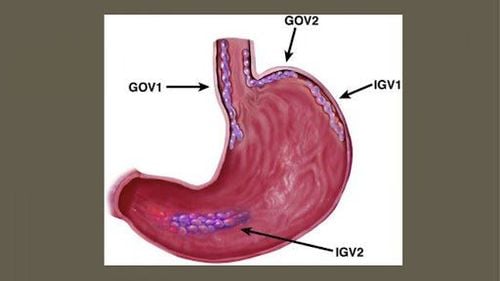
Gastric varices are common varicose veins in the distal esophageal and gastric aneurysms caused by portal hypertension, often present in patients with cirrhosis. Gastric varices can lead to large amounts of gastrointestinal bleeding but are usually not accompanied by other symptoms. Treatment of varicose veins is mainly by rubber band ligation and intravenous injection of octreotide. Sometimes patients also need surgery to connect the 2 portal veins.
Portal hypertension is the result of a number of diseases, mainly cirrhosis. If portal pressure remains above superior vena cava pressure for a certain period of time, collateral circulation occurs. The most dangerous collaterals occur in the distal esophagus and gastric aneurysm, causing the submucosal vein to become prominent and filled with blood known as varicose veins. These varicose veins partially relieve portal pressure, but can rupture at any time, causing severe gastrointestinal bleeding. The trigger for the rupture of these varicose veins is unknown, but bleeding is almost never expected unless the portal/caval pressure is >12 mm Hg. Coagulation disorders in liver disease can also lead to bleeding more easily.
Gastrointestinal bleeding is the most typical symptom of varicose veins. Bleeding is usually sudden, painless in the upper gastrointestinal tract, and often bleeds in large amounts, which can even shock the patient from blood loss. Bleeding will usually originate in the distal esophagus, less commonly in gastric aneurysms. Gastrointestinal bleeding from gastric varices can be acute but is usually subacute or chronic. In addition, gastrointestinal bleeding may initiate hepatic encephalopathy in patients with impaired liver function.
Chỉ định thắt tĩnh mạch phình vị trong việc xử trí ca bệnh xuất huyết tiêu hóa
2. Diagnosis and prognosis of gastric aneurysms
2.1. Diagnosis of varicose veins
Diagnosis of gastric aneurysm is mainly based on endoscopy and assessment of coagulation status.
Both gastric and esophageal varices are diagnosed endoscopically and are both high risk factors for gastrointestinal bleeding (eg, in patients with vascular score).
Endoscopy is also important to rule out other causes of acute bleeding (such as peptic ulceration), even in patients with pre-diagnosed varicose veins, at least Approximately one-third of patients with varicose veins develop gastrointestinal bleeding not due to varicose veins.
Because varicose veins are often associated with liver disease, evaluation of coagulation status is essential. Tests include a complete blood count, specifically platelets, PT, APTT and liver function tests. Patients who are bleeding should have their blood group tested and cross blood for 6 units of red blood cell mass.
2.2. Prognosis
In approximately 40% of patients with gastrointestinal bleeding due to gastric aneurysms, the bleeding stops spontaneously. In the past, mortality was >50%, but even with current treatments, mortality is still over 20% at 6 weeks. The mortality rate depends mainly on the severity of the patient's liver disease rather than on the current bleeding. Bleeding is often fatal in patients with severe liver failure (eg, advanced cirrhosis), whereas patients with well compensated liver function usually recover.
Survivors have a high risk of recurrent bleeding, typically, 50 to 75% of cases relapse within 1 to 2 years. Endoscopic or medical therapy is significantly reducing this risk, but the overall effect on long-term mortality appears to be negligible, possibly due to underlying liver disease.

Xuất huyết tiêu hóa là triệu chứng điển hình nhất của giãn tĩnh mạch phình vị
3. Indications for varicose vein ligation
Gastroesophageal varices bleeding is one of the major complications caused by portal hypertension in patients with cirrhosis. Although the risk of bleeding from gastric varices is lower than that of esophageal varices, if present, the consequences are more severe, the mortality rate is higher, and the risk of rebleeding is also high. than. The estimated mortality rate for gastrointestinal bleeding from gastric varices would be approximately 55 percent.
Most gastric varices drain into the left renal vein, then into the inferior vena cava, and then through the gastro-renal shunt (GRS). The existence of this connection can also cause another serious complication, which is hepatic encephalopathy, because undetoxified blood is dumped directly into the systemic circulation instead of the liver.
Today, there are many methods to treat bleeding caused by gastroesophageal varices, in which endoscopic variceal ligation and sclerotherapy are the first indications. BRTO (balloon-occluded retrograde transvenous obliteration) is a vascular interventional technique that mistakenly blocks gastric varices and closes the portal shunt. This method has many advantages such as safety, high success rate, low rebleeding rate, improved liver function (improved portal venous flow to the liver), can be indicated for patients. have hepatic encephalopathy and impaired function.
However, the main disadvantage of BRTO is that it only locally resolves the gastric varices and does not resolve portal hypertension. In addition, the occlusion of the portal shunt will increase the risk of esophageal varices rupture. Technically, BRTO has the disadvantage of having to store the blocker in the catheter for a long time (from 3 to 12 hours). This will lead to many risks such as bleeding at the puncture site, infection, thrombosis, balloon rupture and inconvenience to the patient.
Currently, BRTO has been replaced by PARTO (plug-assisted retrograde transvenous obliteration). The PARTO method using the amplatzer vascular plug allows the occlusion of large-diameter blood vessels in a short time, thus overcoming the disadvantages of BRTO.
Gwon's study showed that 98.6% of cases had complete thrombosis of varicose veins and catheterization without complications. According to the latest recommendations in 2020 of the Korean Hepatobiliary Association, PARTO is the first choice technique for the treatment of gastrointestinal bleeding due to varicose veins of the fundus besides sclerotherapy and TIPS.
In addition to the indications for varicose vein ligation, gastrointestinal bleeding due to varicose veins can also be treated with the following methods:
Rehydration, blood transfusion if the patient loses too much blood Rubber band ligation Injection intravenous octreotide Surgical anastomosis (TIPS) Fluid resuscitation, including blood transfusion if necessary, is performed to manage hypovolemic and hemorrhagic shock. Patients with coagulation abnormalities (eg, the INR may be significantly increased) can be treated with 1 to 2 units of fresh frozen plasma, but caution should be exercised because the administration of large volumes of fluid to Patients who are not hypovolemic may actually have an increased risk of bleeding from the varicose veins. Patients with cirrhosis with gastrointestinal bleeding are at risk for infection and should receive antibiotic prophylaxis with norfloxacin or ceftriaxone.
Because varicose veins are diagnosed endoscopically, endoscopy is the initial treatment. Laparoscopic rubber band ligation is more applicable than sclerotherapy. At the same time, intravenous administration of octreotide was also made (a synthetic analogue of somatostatin). Octreotide increases vascular resistance by inhibiting the release of mediators that induce vasodilation (glucagon, vasoactive peptide peptide). The usual dose is an intravenous bolus of 50 mcg, followed by an intravenous infusion of 50 mcg/h. Octreotide is preferred over previously used analogues, such as vasopressin and terlipressin, because it has fewer side effects.
If bleeding continues or recurs despite the above measures, perform an emergency procedure to return blood from the portal venous system to the vena cava to relieve portal pressure and reduce bleeding. . TIPS is an invasive radiographic procedure in which a wire is inserted from the vein through the liver parenchyma into the portal vein system. The anastomosis is then balloon dilated and a metal catheter (stent) inserted to create a bridge between the vena cava and the hepatic vein. Stent size is important. If the stent is too large, it can lead to hepatic encephalopathy due to too much blood from the portal vein. If the stent is too small it is more likely to become blocked again. Portal vein bypass surgery, such as splenic-renal venous shunting, works by a similar mechanism but is more invasive and carries a higher mortality rate.
Use of Sengstaken-Blakemore catheters or other types of catheters can increase mortality and is generally not considered optimal treatment. However, the use of this catheter can be a temporary solution in the case of waiting for TIPS or surgery. The Sengstaken - Blakemore catheter is a flexible nasogastric tube with a balloon inserted in the stomach and a balloon inserted in the esophagus. After insertion, the intragastric balloon is inflated with a fixed volume of air, and then traction is applied to the tube to pull the balloon snugly against the gastroesophageal junction. This balloon is usually sufficient to control bleeding, but if not, the esophageal balloon is inflated to a pressure of 25 mm Hg. The procedure is quite uncomfortable and can lead to perforation and reflux into the airways; therefore, intubation and intravenous anesthesia are usually recommended.
Liver transplantation can also reduce portal hypertension but this is an option only for patients already on the transplant list.
Long-term therapy of portal hypertension (with beta-blockers and nitrates) is discussed elsewhere. Treatment of portal-related hepatic encephalopathy may be necessary.
Splenectomy is performed to treat gastric bleeding due to splenic thrombosis (sometimes as a result of pancreatitis).
Thus, gastric varices are the main cause of gastrointestinal bleeding, especially in patients with cirrhosis. The severity of liver disease is a major determinant of patient mortality during an episode of gastrointestinal bleeding. The recurrence rate is quite high, about 50-70% in the first 1-2 years. Varicose veins are a dangerous disease, so those at high risk, especially those with liver disease, should have regular checkups to be able to detect early and treat the disease in time.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.