This is an automatically translated article.
The article was professionally consulted by Dr. Tran Nhu Tu - Dean and Master, Doctor Nguyen Thanh Nam - Department of Diagnostic Imaging - Vinmec Danang International General HospitalInfertility is not only a medical gynecological disease, but it also has a great influence on sociological issues. In women in Vietnam, the secondary cause of infertility due to tubal occlusion is more than 70%. Hysterosalpingography - hysterosalpingography is currently a highly valuable method in diagnosis and treatment.
1. Hysteroscopy - what is the fallopian tube?
Hysterosalpingography – tubal angiography (TC-VTC) is a survey of the uterine cavity and two fallopian tubes by contrast injection after catheter placement in the cervical opening. Then use an X-ray machine to produce images for diagnosis.2. Indications and contraindications for the method
Is a hysterosalpingogram harmful? As a method that uses X-rays but with a very low dose of radiation, hysterosalpingograms are very helpful in detecting reproductive-related diseases, especially infertility.Indicated in the following cases
Patients with infertility Patients with uterine mass, endometriosis or uterine malformation. Check for a non-contrast IUD. Contraindicated in the following cases
Absolute cases
Pregnant women: The technique is performed at the beginning of the menstrual cycle In case of suspected pregnancy beta HCG should be tested Adnexal infections: In case of doubt, blood count, erythrocyte sedimentation rate and tubal stasis should be checked by ultrasound. Relative case
Existing heavy bleeding The patient is on an IUD

Phụ nữ đang mang thai tuyệt đối không chụp tử cung vòi trứng
3. What does the patient need to prepare before the procedure?
Provide enough information for the doctor to perform, prepare psychologically and cooperate as much as possible during the working process. Testing should only be done 4-8 days after the female patient has had a period. Stop taking and use the drug. Contrast drugs in use Some exceptions
Patients with a history of infection should take antibiotics 3 to 5 days before and after the test; Patient anxiety and stress during the scan: use mild analgesics; History of spasms: antispasmodic before 2 hours and 15 minutes; Menopausal women: for patients to use estrogen daily and continuously for 8 days to increase nutrition for the vagina and cervical canal; Women on oestro-progestal therapy, taking oestrogen-phase scans.

Kỹ thuật chụp tử cung - vòi tử cung được thực hiện sau 4-8 ngày sạch kinh
4. Steps to perform a hysteroscopy - tubal scan
Unprepared abdominal filmLocalized subframe with the aim of finding areas of calcification and contrast.
Place speculum after vaginal examination
Have the patient urinate before the procedure; Place patient in supine position with legs elevated; Vaginal examination to determine the volume and position of the uterus and cervix; Disinfect the vulva, spread sterile towels; Place the speculum in a suitable position, gentle manipulation without pain, allowing cervical examination. In the case of vaginal discharge or ectopic cervicitis, the test must be postponed. Place the metal instrument on the cervix
Disinfect the cervix before inserting the instrument Measure the uterine cavity with a ruler then choose a rubber cone (or metal cone) so that the size is suitable for the external hole cervix to attach to the instrument; Disinfection of hysterosalpingogram instruments; Fill the tube with contrast agent, push out all the air bubbles in the tube; Clamp the Pozzi to the lateral border of the cervix in the vertical direction (use 1 or 2 depending on the case); The cone attaches to the imaging device and is then inserted into the ectopic opening of the cervix. Pozzi clamps are fixed to the tool. We adjust the instrument so that the cone fits snugly against the cervix to avoid contrast reflux.
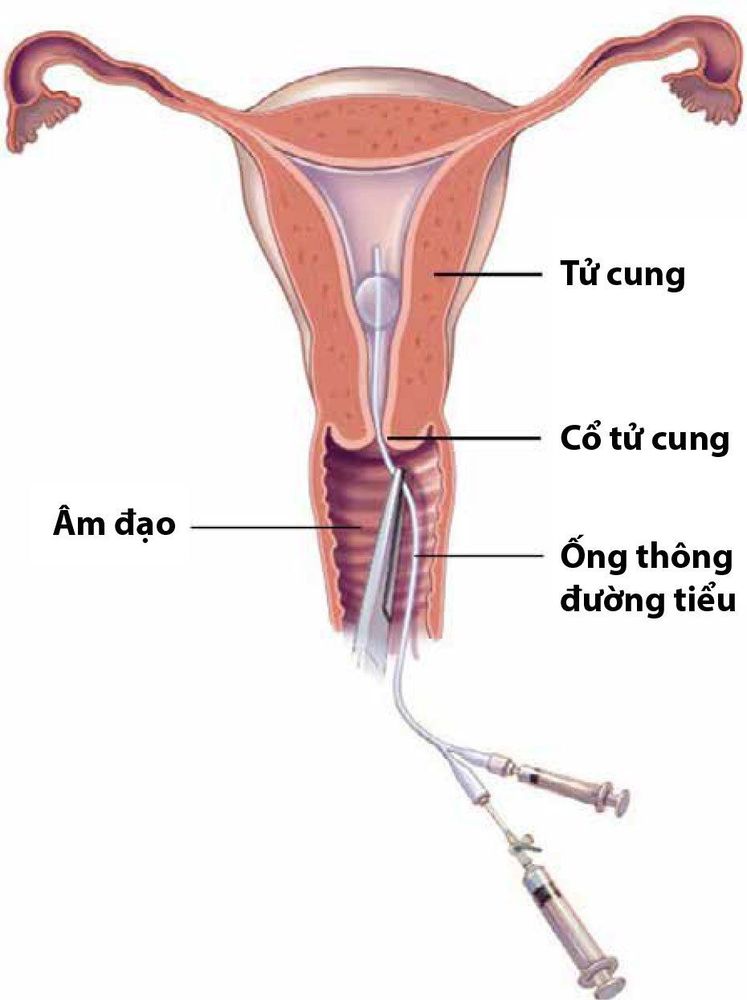
Thực hiện kỹ thuật chụp tử cung - vòi tử cung
Inject the contrast agent into the uterus
Inject a few mL of the contrast agent and examine the position of the instrument under the screen; The speculum can be removed prior to film shooting to avoid obscuring the image of the camera; The doctor pulls the cervix while injecting the contrast agent gently, intermittently. Simultaneously, monitor and check under the light of the instrument position, the uterine cavity is full, the contrast agent is passed through the tube to the peritoneum, the contrast agent is refluxed into the blood vessels, the uterine mobility; In case the contrast agent does not enter the peritoneum on one or both sides, we increase the injection pressure based on the manometer (no more than 200mmHg) attached to the instrument or based on the patient's pain sensation, maintaining pressure. this high for a period of 5 minutes. Film locations
Film straight thin layer of the uterus; Film taken straight filled with uterine cavity and two tubes, drug into the peritoneum; Tilting film of the uterus filled with contrast medium to view the neck, waist, and body of the uterus; Bilateral oblique film is performed infrequently, viewed when the fallopian tubes overlap, the cervical-coastal axis of the uterus is flexed; A straight film may be taken during cervical traction to examine the cervix. Remove contrast agent
First, remove Pozzi clamp and stop bleeding at Pozzi clamp position with sterile cotton and gauze; Take a film immediately to see the cervical region; It is possible to take the film late, put the patient on the stomach after about 15 minutes of walking. Searching for the stagnation of contrast agent in the uterine cavity and fallopian tubes; In the case of tubal stasis, check with a standing scan after 24 hours, continue antibiotics for a few days after the scan. Cotte test
Positive Cotte test: Contrast is released in the peritoneal area when the film is full or in the late film after 15 minutes.

Kết quả chụp tử cung - vòi tử cung
5. Evaluation of results
The results of hysteroscopy - the fallopian tubes clearly show the anatomical structures of the uterus and fallopian tubes, the two tubes are filled with contrast; Through the displayed image, it is possible to detect damage to the cervical area if any.6. Handling of complications during hysteroscopy - fallopian tubes
After hysteroscopy, there will be some complications. Here are some notes after taking hysterosalpingogram and how to handle it when there is an accident:Management of contrast agent complications: Follow the procedure of Diagnosing and dealing with Contrast Contrast Complications by the Ministry of Health. Health issue and licensing; The patient has pelvic pain after the scan: This is caused by the pressure during contrast injection, which can be avoided if antispasmodics are used. But if there is pain in the pelvic area after the scan, it is very likely to have an infection; Contrast reflux into blood vessels: less important, but easy to react with contrast intolerance; Uterine perforation: Extremely rare; Bacterial infection: very rare if the scan steps are done properly; If tubal stasis is present, antibiotics should be continued for a few days after the scan. A hysterosalpingogram (HSG) is the method used to diagnose abnormalities of the uterine lumen and circulation. and tubal morphology. Currently, the method is mainly indicated in cases of suspected obstruction or dilation or abnormality of the fallopian tubes causing infertility. Indications can be made depending on the assessment of the gynecologist or the doctor who is treating the client's infertility. Besides, you need to note, hysterosalpingogram should make an appointment from 2 to 5 days after the menstrual period to be able to conduct the scan.
Currently, Vinmec International General Hospital conducts HSG scans according to technical procedures that meet the standards of the Ministry of Health, ensuring patient safety according to international standards. Synchronous camera system, modern equipment and standard, sterile imaging room. Professional and experienced doctors and technicians help diagnose and give the most accurate results to patients in a short period of time. In particular, customers who book an appointment before coming to the hospital will be examined immediately because they are fully prepared without having to wait. With the above conditions, you can completely trust the quality of medical services at Vinmec