This is an automatically translated article.
Among all types of tuberculosis, pulmonary tuberculosis is quite common due to its high prevalence. However, there are other forms of extrapulmonary tuberculosis that also need to be detected and diagnosed so that it can be treated promptly and appropriately, bringing high treatment efficiency. Such classification of the disease is intended to help accurately diagnose whether it is pulmonary or extrapulmonary tuberculosis, from which appropriate treatment measures can be taken. The best way to prevent TB is to get vaccinated in the first months of life.1. Classification of tuberculosis according to anatomical location
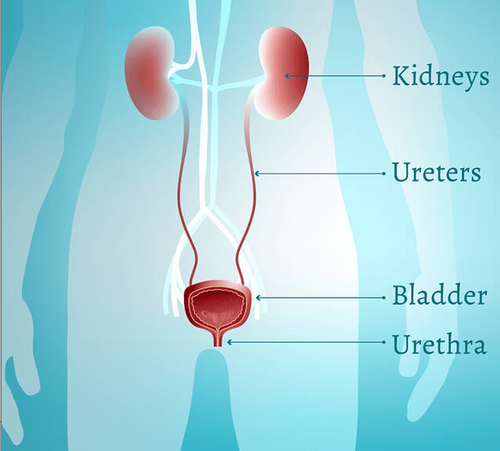
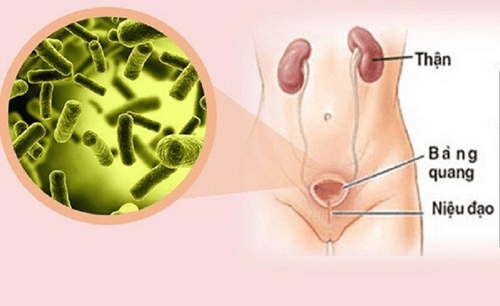
Tuberculosis is classified according to anatomical location, including:Pulmonary tuberculosis: is a tuberculosis bacteria that damages the lungs and bronchi, including millet tuberculosis. However, if there is a combined lesion in both the lungs and extrapulmonary organs, they are collectively classified as pulmonary tuberculosis. Extrapulmonary TB: is a tuberculosis bacterium that damages organs outside the lungs such as pleura, lymph nodes, peritoneum, genital and urinary organs, skin, bones, joints, pericardium, meninges, etc. In the case of tuberculosis in many parts, but which part has the most severe damage such as tuberculosis of the meninges, tuberculosis of bones, or tuberculosis of joints... is determined as the main diagnosis. 1.1. Classification of pulmonary tuberculosis according to the results of the direct smear test In pulmonary tuberculosis, the classification according to the results of the direct smear test includes:
Pulmonary tuberculosis with AFB (acid fast bacilli) positive (+). Pulmonary tuberculosis has negative (-) AFB (acid fast bacilli) results.

Lao phổi là bệnh phổ biến
Tuberculosis of the lymph nodes: common in the neck. The lymph nodes are enlarged, firm texture, movable, painless, but then the lymph nodes stick together and become less mobile, and the lymph nodes may become soft and leak pus. Lymph node tuberculosis can be cured but will leave bad scars. Pleural effusion due to tuberculosis: the common clinical symptoms of the disease are chest pain, shortness of breath with increasing severity, conducting lung examination, there is a reduced syndrome 3. The pleural ultrasound showed fluid. Tuberculosis causing pericardial effusion: clinical symptoms of the disease depend on the volume and rate of fluid formation in the pericardium. Symptoms of the disease are chest pain, dyspnea, jugular venous distention, lower extremities edema, tachycardia, blood pressure jam, and pulse reversal if there is acute compression syndrome. A pericardial rub is heard in the early stages or a faint heart sound when the effusion is large. Chest X-ray film shows a large heart, teardrop shape, double border. Ultrasound showed pericardial fluid. Tuberculosis causes peritoneal effusion: palpation of the abdomen shows lumps and hard masses. The lymph nodes adhere to the intestine causing obstruction or semi-obstruction. Abdominal ultrasonography showed images suggestive of peritoneal tuberculosis such as enlarged mesenteric lymph nodes, retroperitoneal lymph nodes, and localized fluid between the adhesions. Laparoscopy can show tubercular granules. Tuberculosis meningoencephalitis: clinical symptoms of meningitis usually begin with signs of increasing headache and impaired consciousness. Examination revealed a stiff neck and Kernig was positive. Injury to cranial nerves and focal nerves, circular muscle disorders. Spinal cord injury causes paralysis of the lower extremities. Tuberculosis of the joints: common in the spine with symptoms such as back pain, limitation in movement, pain in the vertebrae damaged in the early stages. In the late stages, the disease causes kyphosis or paralysis due to spinal cord compression. Urinary-genital tuberculosis: common clinical symptoms are urinary disturbances such as dysuria, frequent urination, and remission after antibiotic treatment, but there is recurrence, blood in the urine may be absent. Blood clots, cloudy urine, dull low back pain. In men, genital tuberculosis can cause painful swelling of the testicles and epididymis; however, acute inflammation or epididymitis is rare. In women, genital TB can cause pathological vaginal discharge or vaginal discharge, menstrual disorders, which in the long run can lead to amenorrhea and infertility. Some other uncommon forms of extrapulmonary tuberculosis such as skin tuberculosis, spleen tuberculosis, liver tuberculosis...
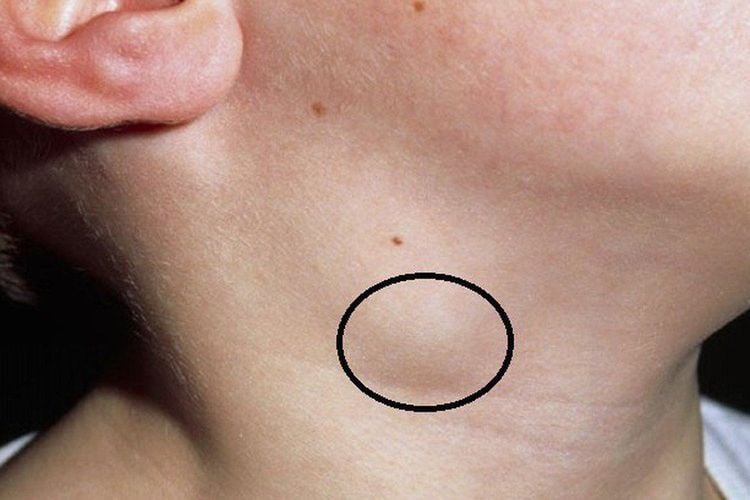
Bệnh lao hạch
2. Tuberculosis classification according to bacteriological test results
Tuberculosis classification according to bacteriological test results includes:
Persons with TB with bacteriological evidence: are patients with at least one of the tests such as direct sputum smear, culture or test WHO-certified TB bacteria such as Xpert MTB/RIF (Mycobacterium tuberculosis/Rifampicin), HAIN (GenoType MTBDRplus) tested positive. Person with tuberculosis without evidence of bacteriology or clinical diagnosis: is a patient diagnosed and treated for TB by a clinician but does not meet the criteria for bacteriological evidence. If TB bacteria are found during subsequent treatment by laboratory tests, the patient is reclassified as having bacteriological evidence.
3. Classification of tuberculosis according to the history of TB treatment
Classification of TB according to the history of TB treatment includes:Newly acquired TB: a patient who has never used anti-TB drugs or has used anti-TB drugs for less than 1 month. Recurrent TB patient: is a patient who has been treated for TB and is determined by the doctor to be cured or has completed treatment, but re-infected with a positive AFB result, or has a medical certificate. bacteriological evidence through testing. Patients with tuberculosis who have failed treatment include: Patients with positive AFB results from the 5th month of treatment or more and must switch treatment regimens; The patient had an initial diagnosis with negative AFB, but after 2 months of treatment, a positive AFB result appeared; Patients with extrapulmonary tuberculosis develop additional pulmonary TB with positive AFB results after 2 months of treatment; Patients with multidrug resistance, identified at any time during treatment with a first-line anti-TB drug. Patients with tuberculosis who are re-treated after stopping treatment: are patients who have not used the drug continuously for more than 2 months during treatment, then the patient returns to treatment and finds AFB positive or has a positive result. bacteriological evidence through testing. Other TB patients include: Pulmonary TB with another positive AFB result: a patient who has received TB drug treatment before with a duration of treatment lasting more than 1 month but the regimen cannot be determined and the outcome is unknown. Results of treatment, or unknown treatment history, is now diagnosed with pulmonary TB with a positive AFB result. Pulmonary TB with negative AFB results and other extrapulmonary TB: is a patient who has been previously treated with anti-TB drugs for a duration of more than 1 month but the treatment regimen and outcome are unknown, or who were on a regimen with assessment as completion of treatment, or with unknown treatment history, now diagnosed with AFB-negative TB or extrapulmonary TB. Person with tuberculosis transferred from another place: is a patient transferred from another treatment unit to continue treatment.

Điều trị bệnh lao phổi theo chỉ dẫn của bác sĩ
4. Classification of tuberculosis according to HIV infection status
Classification of tuberculosis according to HIV infection status includes the following cases:
HIV-positive TB patient: is a patient with HIV-positive test results. HIV-negative TB patient: means the patient has a negative HIV test result. Of note, patients who were initially HIV-negative but later tested HIV-positive should be reclassified. Person with tuberculosis of unknown HIV status: is a patient without HIV test results. These patients need to be reclassified after HIV test results are available.
5. Classification of tuberculosis according to drug resistance
According to the World Health Organization (WHO), TB classification according to drug-resistant status includes:People with prescription-resistant TB: are patients who are resistant to only one first-line anti-TB drug other than rifampicin. Patients with multidrug-resistant tuberculosis: are patients who are resistant to 2 or more first-line anti-TB drugs but are not resistant to rifampicin. In which, patients with tuberculosis resistant to rifampicin are resistant or not resistant to other concomitant TB drugs; may be prescription resistance, multidrug resistance, multidrug resistance or super resistance.
Patients with multidrug resistant tuberculosis (MDR-TB) are resistant to at least 2 anti-tuberculosis drugs, isoniazid and rifampicin. Patients with super-resistant TB have additional resistance to any of the fluoroquinolones or to at least one of the three second-line injectable drugs, such as Capreomycin, Kanamycin, and Amikacin, but not both. Patients with super-drug resistant TB (XDR-TB) have additional resistance to any of the fluoroquinolones and to at least one of three second-line injectable drugs such as Capreomycin, Kanamycin, and Amikacin. Patients with MDR-TB according to treatment history: including cases of new MDR-TB patients, relapse, failure of treatment with formula I, failure of treatment with formula II, re-treatment after quitting treatment. , other multi-resistant tuberculosis. Patients with multi-resistant TB according to pre-treatment tests: include cases S+, C+; S-, C+ and S+, C-.
6. Tuberculosis classification according to treatment history
According to the new classification of WHO, TB according to treatment history includes:
New TB patient: a patient who has never used anti-TB drugs or has been taking anti-TB drugs for less than 1 month. Re-treated TB patients: are patients who have used anti-TB drugs for more than 1 month; There may be relapse, treatment failure, or re-treatment after discontinuing treatment or re-initiating another treatment. Patients with tuberculosis of unknown treatment history
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.