This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalHemorrhagic ulcerative colitis is a chronic inflammatory bowel disease affecting the colon with an unclear pathogenesis. So how is ulcerative colitis found and how does the disease arise?
1. History of bleeding ulcerative colitis
Hemorrhagic ulcerative colitis is a chronic inflammatory bowel disease affecting the colon with an unclear pathogenesis.
The term "bleeding ulcerative colitis" was first used in the literature in the mid-nineteenth century by physician Samuel Wilkes when describing a case of a young woman who died of acute diarrhea with mucosal injury to the entire colon extending to the terminal ileum was severely ulcerated. A few years later, the term was used by pathologists in a study describing the histopathology of 200 patients with bleeding ulcerative colitis. Subsequently, Wilkes and Mozon, as well as many other scientists, tried to differentiate this pathology from other gastrointestinal infections.
W. Hale-White - a British doctor described bleeding ulcerative colitis as a progressive mucosal inflammation that leads to ulcers of varying degrees from the ileal region to the anal canal, at least when there is damage to the ileum.
2. Relationship between clinical symptoms and treatment process
The relationship between clinical symptoms and treatment has been described since 1909 in 300 patients with ulcerative colitis with bleeding and recorded a relatively high mortality rate. Over 50% of patients died from complications such as perforation, peritonitis, gastrointestinal bleeding, infection, pulmonary embolism, liver disease, malnutrition. An interesting point that research has raised is finding the occurrence of this pathology in families with members of the disease. Following that, many case reports in different regions of the world recorded an increasing rate of detection of bleeding ulcerative colitis along with many associated extra-gastrointestinal manifestations such as hepatitis, skin lesions. , match. In 1963 - 1964, Edwards and Truelove described the course of hemorrhagic ulcerative colitis and found predictive factors for mortality including severity, extent of lesions, and age 60 and older.
3. History of pathogenesis
The pathogenesis of ulcerative colitis has not been elucidated so far. However, factors that have been identified to play a role include bacterial infection, genetic factor 70, allergies, and autoimmune mechanisms. In particular, the autoimmune mechanism was first mentioned by the authors Kirsner and Goldgraberg in the period of 70 years from 1930 to 1940, when cases of onset of diseases related to allergies or other diseases were recorded. autoimmune and responsive to steroid treatment.
By 1959, Broberger and Perlmann found the presence of e hemagglutinin antibodies in the colonic mucosa of pediatric patients with bleeding ulcerative colitis. This has opened up many new research directions on the pathogenesis of hemorrhagic ulcerative colitis. In the last 70-80 years, the treatment of ulcerative colitis has undergone significant changes and developments, helping to reduce mortality and improve the quality of life of patients. With the application of biological products, the goal of treatment is to optimize and thoroughly treat this pathology.
4. Is ulcerative colitis bleeding common?
According to a meta-analysis of 147 IBD studies in 2017, the regional prevalence of bleeding ulcerative colitis ranged from 0.5 to 24.5 per 100,000 people. However, there are regions such as Southeast Asia, including Vietnam, which lack epidemiological data. Longitudinal follow-up studies in Western countries have noted that over the past 10 years, the incidence of this disease has increased gradually and earlier than that of Crohn's. Similarly, in developing countries, bleeding ulcerative colitis is more common than Crohn's.
In the Asia-Pacific region, a multicenter study (ACCESS study) was conducted in 21 centers in 12 cities in 9 countries over the span of one year from 2011 to 2012 recording in 419 new cases of IBD, ulcerative colitis with bleeding accounted for 232 cases (55.4%). Annual incidence and age-adjusted incidence rates vary from country to country, with the lowest incidence in some regions of China and Thailand
Also according to this study, in the Asian region, The most common age at diagnosis of ulcerative colitis was from 30 to 34 years old and the disease was more common in men, accounting for 57.9%. When comparing disease progression in Asian and Western patients, data from several studies suggest that disease progression is likely to be milder in Asia and less common in fulminant patients than in patients with fulminant disease. with Western countries.
5. Pathogenesis of ulcerative colitis with bleeding
Until now, although the pathogenesis of bleeding ulcerative colitis is not really clear, the most mentioned hypothesis is that the pathological condition is caused by many factors, including genetic factors. Transmission, environment, and intestinal microbiota affect inappropriate inflammatory responses.
The mechanisms that have been identified include:
Disturbances of the gut microbiota with depletion of beneficial bacterial strains, especially Firmicutes and Bacteroidetes leading to colonic mucosal colonization of viable bacteria. Harmful, increased expression of Toll-like receptor TLR-4 Accumulation of glycosylated precursors of mucin leads to poor quality of intestinal mucus secretion (impaired barrier) Dendritic cells carrying CD10 antigen releases TL27 that activates differentiated immature CD4 T cells and natural killer cells. CD4 T cells differentiate into Regulatory T and Assist Breathing T cells that further produce eosinophil activators. Activated natural killer cells produce IL-13, which destroys epithelial cells, changes the function of the intercellular junction, causes fibrosis, and IL-23, which activates Th7 cells. IL17 production which in turn induces neutrophil chemotaxis Activation of B cells that produce antibody words
6. Clinical manifestations of the disease
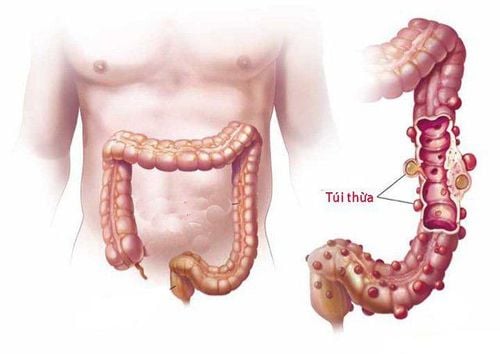
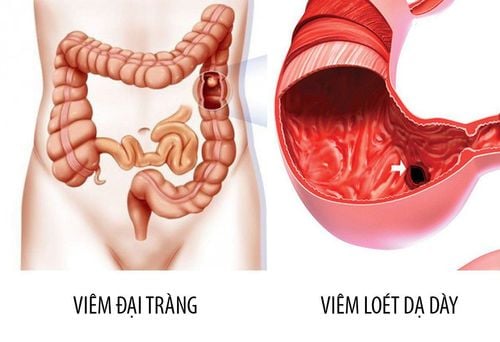
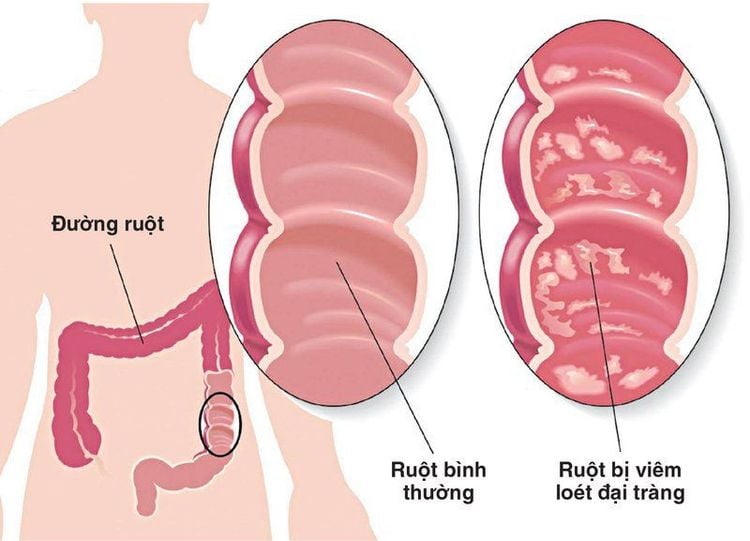
Hemorrhagic ulcerative colitis is characterized by diffuse and superficial inflammatory lesions of the colonic mucosa, beginning in the rectum and extending to other segments of the colon. The small intestine is usually not affected, although the terminal ileum may have superficial inflammatory lesions. Based on the extent of colonic lesions, ulcerative colitis can be classified into the following types: Proctitis (localized lesions in the rectum), sigmoid colitis - rectum or left colon. (spread to the splenic angle) or diffuse/global colitis. The extent of damage is not only related to severity but also affects money and choice of treatment. Symptoms and course of the disease are related to the extent and severity of inflammatory lesions. Symptoms are often insidious, although the disease may develop acutely after an episode of infectious colitis or travel diarrhea. Proctitis causing bloody stools is the most common symptom of patients. The degree of bloody stools can be severe or moderate, bloody stools with mucus. The patient may have frequent urge to defecate and strain or increase the frequency of defecation. The more widespread the colonic damage, the more severe the diarrhea, while if the patient is simply proctitis, symptoms may alternate between episodes of constipation with episodes of bloody stools. Abdominal pain before defecation or a feeling of bloating will be experienced when the disease is advanced. In advanced or fulminant cases, patients may present with systemic symptoms such as night sweats, fever, vomiting, nausea, weight loss accompanied by diarrhea. In addition, there may be extra-gastrointestinal symptoms such as in the eyes, skin, joints, liver.
Up to now, there is no specific medicine that completely cures bleeding ulcerative colitis. Only treatment can help limit the disease, reduce pain for the patient. Therefore, in addition to the treatment prescribed by the doctor, the patient needs to follow a good diet for the digestive system, avoid stress and need to have regular health checkups.
As soon as there are symptoms, it is necessary to go to the doctor soon for timely treatment when the damage has not spread. Vinmec International General Hospital with a team of highly qualified doctors, along with modern medical equipment and international standards, readers can trust to choose as a destination for examination and treatment. for yourself and your family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
The article references the source: NagreF, Gionchetti PR, Eliakim R., De Dombal F.T. (1968), Ulcerative colitis: definition, historical background, Lichtenstein G.R., btv. (2014), Medical Therapy of Ulcerative Colitis, Springer-Verlag, New York.