Article by Master of Medicine, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Anal skin tags are benign and common. Anal skin tags look like small bumps or raised areas on the anus. There can be multiple anal skin tags at the same time. Although anal skin tags can be sensitive, they are rarely painful. However, they can be very uncomfortable and itchy. So how to identify and remove anal skin tags?
1. What causes anal skin tags?
The skin around the anus is often more sensitive than the skin on other parts of the body. This is because the skin in the anal area needs to stretch when having a bowel movement. If a blood vessel near the anus swells or enlarges, it can lead to a wound on the skin. This is because the excess skin tag remains even after the swelling has gone down.
The most common causes of anal skin tags are:
- Straining during bowel movements due to constipation
- Diarrhea
- Heavy lifting
- Strenuous exercise
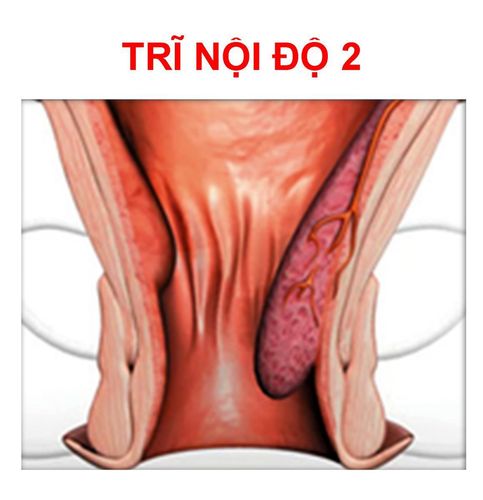
- Hemorrhoids
- Pregnancy
- Blood clots
If patients have hemorrhoids or other vascular conditions around their anus, they may be more likely to develop anal skin tags.
The skin may form due to inflammation if patients have Crohn's disease or another inflammatory condition. In a review article on the condition, up to 37% of people with Crohn's disease develop anal skin tags.
2. How are anal skin tags diagnosed?
Although anal skin tags are benign, they can still be a cause for concern. That's why it's important to see your doctor to confirm that the swelling or bulge you feel is the result of a skin injury and not a tumor or blood clot.
To make a diagnosis, your doctor will likely perform a physical exam. During the exam, you may be asked to remove your underwear and lie on your side. Your doctor may perform a visual examination and look at your anus for signs of skin lesions. They may also perform a rectal exam and insert a finger into your rectum to feel for lumps or bulges.
If your doctor needs more information to make a diagnosis, they may also use one of two procedures to look inside your anus and rectum. Both anoscopy and sigmoidoscopy can help rule out any underlying anorectal conditions or concerns, such as cancer.
Your doctor may also take a tissue sample or biopsy and send it to a lab for testing.
Once a diagnosis is made, your doctor can begin discussing your treatment options. Sometimes removal of the anal skin tag may be recommended, but in some cases, no intervention is needed. This will depend on the appearance and cause of the anal skin tag.

3. What to Expect During Anal Skin Tag Removal
Anal skin tag removal is usually a procedure performed in the operating room or a minor surgery room. Anal skin tags are located outside the anus and can be easily reached and removed by your doctor.
For this procedure, your doctor will inject an anesthetic around the skin to reduce pain. You may also be given a sedative to help you relax. Before removing the skin tag, your doctor will clean the area with antibacterial soap.
The procedure for removing anal skin tags is quick and simple. Your doctor will use a scalpel to cut away the excess skin, then use absorbable sutures or staples to close the incision.
Some doctors may use a laser or liquid nitrogen instead of surgical removal. Cryotherapy, using liquid nitrogen, freezes the skin. Over a few days, the excess skin will fall off. The laser burns away the excess anal skin and any remaining skin falls off.
To prevent complications, your doctor may only remove a portion of the anal skin at a time. This gives the area time to heal and reduces the risk of infection from stool or bacteria.
4. What to expect from aftercare
Recovery from an anal skin removal is quick. After the procedure, you will need to stay home and relax. You should not lift heavy objects or exercise.
You can return to work the next day and resume normal activities within a week.
The doctor will likely prescribe a course of antibiotics to reduce the risk of infection. They may also prescribe an antifungal cream and a topical pain reliever to apply to your anus. These creams can help promote healing and reduce pain or tenderness in the days after the removal.
What will happen during recovery
Recovery from an anal skin removal procedure is usually easy, but it is important to follow your doctor's aftercare advice. Infection can delay healing and you may need additional treatment to prevent the spread of bacteria.
In the first few days after the procedure, your doctor may suggest you to take laxatives or try an elimination diet. This will make bowel movements easier and reduce the chance of constipation.
Pressure on the anus can cause pain near the removal site. If you are experiencing pain or other discomfort, using a topical pain reliever may help relieve your symptoms.

5. How to Prevent Anal Skin Tag
After anal skin tag removal, talk to your doctor about strategies to prevent future anal skin tags. Being aware of the conditions that can cause anal skin tags can help you avoid them.
Try these home remedies to avoid further anal skin tags:
- Take a laxative or fiber supplement to make stools softer and easier to pass.
- Apply a lubricant or petroleum jelly to the rectum before a bowel movement to help make stools easier to pass.
- Clean and sanitize the anus after each bowel movement to help avoid friction and irritation that can lead to skin injuries.
These measures may not always be enough to prevent anal skin lesions. If you suspect you have this condition or have developed another condition, talk to your doctor to confirm the suspicious spot.
6. Is it necessary to intervene with anal skin tags?
If you develop an anal skin tag, it is probably not a cause for concern. For most people, anal skin tags are just a nuisance. If they do not bother you and you are sure of the diagnosis, you can leave them alone and not intervene. Remember that where you have anal skin tags, other anal skin tags may appear.
Some anal skin tags do not go away. You may need more than one treatment to remove them. If an anal skin tag becomes hardened or flaky, it may take several weeks for the tag to fall off. In some cases, anal skin tags will grow back and need to be removed again.
Conclusion
If you have an area that develops bleeding, itching, or changes color, contact your doctor immediately. They will need to rule out a serious condition such as skin cancer.
Common and harmless — anal skin tags are small bumps on the anus that may feel itchy. Causes include hemorrhoids, diarrhea, and inflammation. Your doctor can remove anal skin tags in a procedure in the operating room. Laxatives and a liquid diet can help with recovery, and lubricants can prevent more tags from forming.
To arrange an appointment, please call the HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.
References
- Bonheur JL, et al. (2008). Anal skin tags in inflammatory bowel disease: New observations and a clinical review. DOI:10.1002/ibd.20458
- Deep vein thrombosis. (2017).medlineplus.gov/deepveinthrombosis.html
- Hemorrhoids. (2017).familydoctor.org/condition/hemorrhoids/
- Mayo Clinic Staff. (2017). Anal fissure.mayoclinic.org/diseases-conditions/anal-fissure/symptoms-causes/syc-20351424
- Safar B, et al. (2007). Perianal Crohn’s disease. DOI:10.1055/2Fs-2007-991027
- Spanos CP. (2012). Anal skin tags: Removal made simple. DOI:10.1111/j.1463-1318.2012.03087.x