This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Eosinophilic gastroenteritis is an eosinophilic infiltrate in the stomach, small intestine, colon, and rectum causing clinical symptoms. Knowing the process of formation and signs of the disease will help improve the effectiveness of treatment.
1. Eosinophilic gastroenteritis
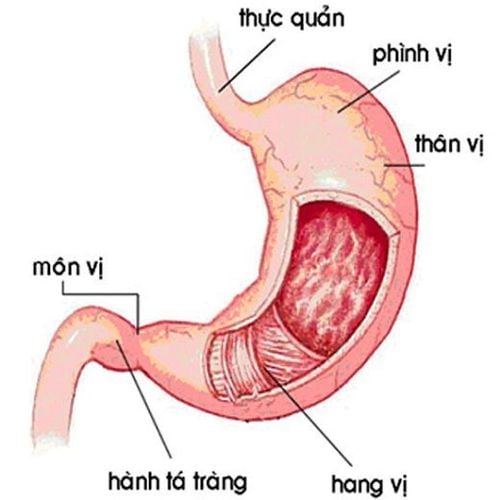
Eosinophilic gastroenteritis is a rare and unusual condition characterized by patchy or diffuse eosinophilic infiltration of the gastrointestinal tract tissue, which was first described. described by author Kaijser in 1937. Each case is unique with specific lesions, depending on the location as well as the depth and depth, extensive spread of the intestine, and chronic recurrence (chronic) relapsing course). The disease can be classified into mucosal (mucosal), muscular (muscular) and serosal types based on the depth of the lesion. Reports are sufficient and damage to almost all digestive organs from esophagus to colon, in which stomach is the most affected organ, followed by small intestine and colon.
Eosinophilic gastroenteritis (English used from Eosinophilic gastroenteritis_EG) is a disease in the following group of diseases: eosinophilic esophagitis (eosinophilic esophagitis), gastritis, enteritis, colitis eosinophil gastritis, enteritis, and colitis), and members of this family of diseases are collectively known as eosinophilic gastrointestinal disorders (EGIDs).
2. How is eosinophilic gastroenteritis found?
The concept of eosinophilic gastroenteritis was first described in 1937 by the author Kaijser, but it was not until 1961 that Ureles et al. first classified this pathology into two types: Diffuse. and localized to form granulomas. In 1970, KLein et al. divided this pathology into three types based on the degree of infiltration of BCAT: mucosal body, myocardium and serosa. By 1985, Oyaizu et al. had found evidence to confirm the role of IgE, mast cell-mediated mechanisms in the pathogenesis of eosinophilic gastroenteritis. Further, case series studies and longitudinal follow-up studies have contributed to further knowledge of the clinical symptoms, histopathology, treatment and course of this rare disease.
3. How is eosinophilic gastroenteritis formed?
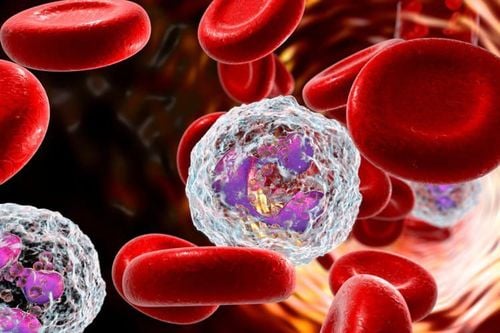
Eosinophils play a major role in the pathogenesis of eosinophilic gastroenteritis. These cells are characterized by eosinophilic staining. In the bone marrow, eosinophils mature and differentiate under the influence of translation factors including GATA-1, GATA-2 and C/EBP. These factors will affect eosinophil growth factors including IL-3, IL-5 and GM-CSF. BCAT stays in the bone marrow for about 8 days, then goes to the peripheral circulation and accounts for 1-3%. After 8 - 12 hours, cells begin to gather to the wall of the digestive tract.
JL-5 is the major chemical mediator of eosinophil activation. Experimental animal studies have documented increased IL-5 production leading to eosinophilia in the peripheral blood. In contrast, with inactivation of the gene encoding IL-5, there was a significant decrease in BCAT in the gastrointestinal and respiratory tracts after allergen exposure.
The migration of eosinophils from peripheral blood into tissue infiltrates is regulated by the chemoking eotaxin-1, eotoxin-2 and b-3. Eotaxin-1 has the role of BCAT concentration and chemotaxis. Experiments in mice have demonstrated that eotoxin-1 deficiency reduces the ability of BCAT to accumulate in the gastrointestinal tract.
Eosinophils are attracted and aggregated in the presence of nonspecific grave injury, antigen exposure or infection. When activated, BCAT releases intracellular granules and produces a number of cytokines including BCAT peroxidase (eosinophil peroxidase), eosinophil-derived neurotoxin (EDN), ECP protein and the major basic protein (MBP). These substances have cytotoxic effects on epithelial cells, stimulate mast cells and basophils to release intracellular granules, and stimulate intestinal M2 muscarinic receptors.
In addition, some other chemical mediators produced by eosinophils such as leukotrienes have the effect of contracting smooth muscle cells, increasing vascular permeability and mucus secretion; IL-1, IL-3, IL-4, IL-5, IL-6, IL-8, GM-CSF, TGF-3/8, TNF and eotaxin initiate inflammation. TGF-B has been shown to be involved in epithelial cell proliferation, tissue remodeling, and fibrosis formation. EPO can produce large amounts of hydrogen peroxide and halide acid that cause tissue damage. Many studies have found evidence of the deposition of cytokines such as MPB, ECP in the extracellular space of the small intestine mucosa in eosinophilic gastroenteritis. Biopsies from the duodenum in these patients also showed structural changes in eosinophils such as increased intracellular granulation and chemical mediators.
4. Classification of eosinophilic gastroenteritis
Depending on the location of the lesion (where eosinophils enter), people divide eosinophils gastroenteritis into the following types:
Eosinophilic gastritis Eosinophilic small intestine Eosinophilic small bowel gastritis Eosinophilic colitis Eosinophilic proctitis For eosinophilic colitis, mucosal involvement leads to symptoms malabsorption, diarrhea, protein loss. Transmural forms of disease will lead to thickening of the colon wall and cause symptoms of intestinal obstruction. Patients may also have perianal disease, visceral neuropathy, chronic semi-obstruction...
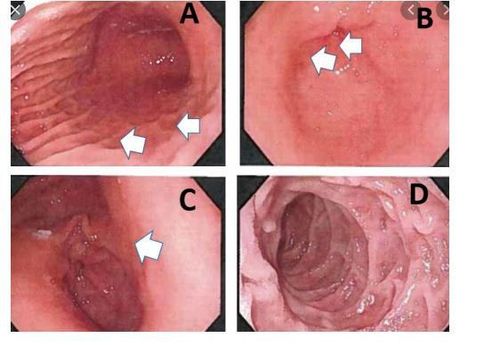
Eosinophilic colitis occurs in breastfed or milk-fed infants cows or soy-based formulas. Symptoms usually present at 2 months of age and include chronic diarrhea with bloody mucopurulent stools. Endoscopy results can show lesions in the form of edema, congestion or lymphatic cysts. Histopathologically, eosinophil and plasma cell infiltrates were seen in the epithelial chorion. Clinical symptoms and histopathology both improved with the use of a dairy-free diet or a formula diet.
Eosinophilic gastroenteritis is an emerging disease and was once considered a rare but increasingly common condition, due to abnormal infiltration of eosinophils into the gastric mucosa, small intestine, The colon affects the structural function of these organs. Clinical symptoms of this disease are also easily confused with other gastroenteritis diseases. Patients with gastrointestinal symptoms should visit specialized facilities for timely diagnosis and treatment.

Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment of eosinophilic gastroenteritis at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References 1. Kaijser R (1937). Allergic diseases of the gut from the point of view of the surgeon. Arch Klin Chir, 188.36-64. 2. Ureles A. L., Alschibaja T., Lodico D. et al (1961). Idiopathic eosinophilic infiltration of the gastrointestinal tract, diffuse and circumscribed; a proposed classification and review of the literature, with two additional cases. Am J Med, 30,899-909. 3. Klein N. C., Hargrove R. L., Sleisenger M. H. et al (1970). Eosinophilic gastroenteritis. Medicine (Baltimore), 49(4), 299-319. 4. Oyaizu N., Uemura Y., Izumi H, et al (1985). Eosinophilic gastroenteritis. Immunohistochemical evidence for IgE mast cell-mediated allergy. Acta Pathol Jpn, 35(3), 759-766. 5. Talley N, J., Shorter R. G., Phillips S. F. et al (1990). Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut, 31(1),54-58.
SEE MORE
Mononucleosis: What you need to know Common dysfunctions in the esophagus and stomach Eosinophils: What you need to know