This is an automatically translated article.
Intubation is a technique used in anesthesia, surgery and especially in emergency resuscitation. This method helps to open, protect the airway and provide the best invasive artificial ventilation.
1. What is intubation?
Intubation is an emergency technique that should be performed on patients who are unconscious or unable to breathe on their own. This technique helps to maintain a clear airway and prevent choking.
The typical intubation procedure is done while you are under anesthesia, then a flexible plastic tube is placed into your windpipe through your mouth to ensure breathing.
The breathing tube used for intubation has many different sizes to suit each patient's age and throat size. The breathing tube will be held in place by a small ring of air that is inflated around the tube once it is in place.
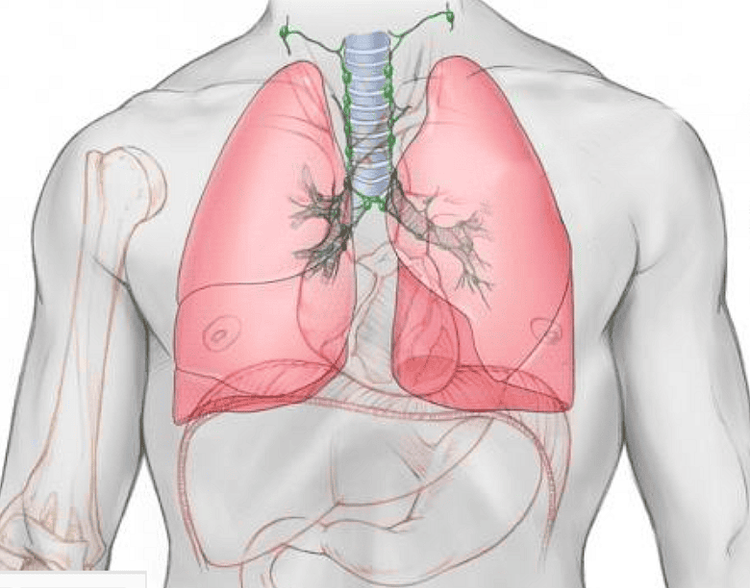
The trachea is an airway that begins below the larynx and extends downward, behind the breastbone. The trachea then divides and becomes two smaller tubes called the right and left bronchi. Each of these main bronchi connects to one of your lungs. The bronchi then further divide into smaller airways in the lungs.
If for any reason your airway from the nose to the trachea is affected leading to shortness of breath or not being able to breathe, then intubation is necessary.
2. Why is endotracheal intubation needed?
Đặt nội khí quản giúp bảo vệ phổi của bệnh nhân
You may need to be intubated for any of the following reasons:
To open your airways for anesthesia, medication, or oxygen. To protect your lungs. You have trouble breathing or can't breathe anymore. You need to use a ventilator. You have a head injury and cannot breathe on your own. You need anesthesia for a long time to have surgery or to recover from a serious injury or medical condition. Intubation keeps your airways clear, which allows oxygen to get to your lungs.
3. How is intubation performed?
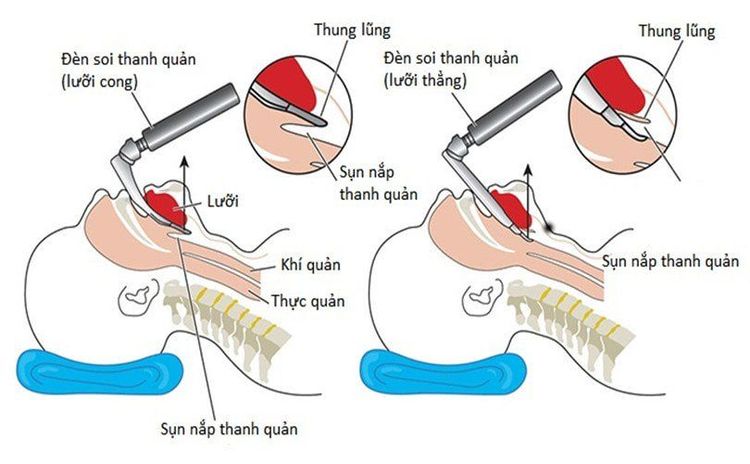
Hình ảnh mổ tả quá trình thực hiện đặt nội khí quản
Intubation is an invasive technique and can cause significant patient discomfort. However, usually patients will be given general anesthesia and muscle relaxants so that they do not feel pain.
But there are also some cases where the technique needs to be performed even when the patient is awake. A local anesthetic can be used to numb the airways to reduce discomfort.
The intubation technique is usually done in the hospital. But in emergency situations, a medical staff can perform intubation right at the place of the patient in distress.
In a typical intubation procedure is done as follows:
The patient will be anesthetized first. When the patient has fallen into a state of anesthesia, the doctor will open the mouth and insert a small tube with a light to look at the larynx. Once the doctor has located the patient's vocal cords, a flexible plastic tube will be inserted from the mouth, through the outside of the vocal cords into the windpipe. In difficult cases, the use of a laryngoscope is necessary, for a more detailed view of the airways.
The doctor then needs to check that the catheter is in place. The endotracheal tube is removed when the patient no longer needs breathing assistance. During surgery and in intensive care, this catheter is connected to a ventilator. After intubation, the patient may experience mild sore throat or difficulty swallowing, but these should go away quickly.

Bệnh nhân có thể gặp phải những triệu chứng đau ngực khi đặt nội khí quản
However, patients may also experience more unpleasant and dangerous symptoms. You should tell your doctor right away if you experience any of the following symptoms:
Swelling of the face Severe sore throat Chest pain Difficulty swallowing Difficulty speaking Neck pain Shortness of breath These symptoms can be a sign of problems different from the patient's airway.
4. What are the possible complications of intubation?
4.1. Complications from anesthesia during intubation Usually, the patient will be under general anesthesia during the intubation process. Therefore, the patient will not feel anything when the catheter is inserted into the trachea.
Healthy people usually don't have any problems with general anesthesia, but there are some small risks and long-term complications. These risks largely depend on the general health of the patient.
Factors that can increase the risk of complications during anesthesia include:
Chronic problems with the lungs, kidneys or heart. Diabetes. Epilepsy. Family history of adverse reactions to anesthesia. Sleep apnea. Fat. Allergies to foods or drugs. Drink alcohol. Smoke. Year old. Serious complications can occur in people who are older and have other medical conditions. Dangerous but rare complications include:
Đau tim biến chứng nghiêm trọng có thể xảy ra ở những người lớn tuổi
Heart attack Lung infection Stroke Temporary mental disturbance Death About 1-2 people in 1000 can be partially awake during general anesthesia. If this happens, the patient is usually aware of their surroundings but feels no pain. These patients may experience severe pain, however this is very rare. This can lead to long-term psychological complications such as post-traumatic stress disorder. Several factors can increase the risk of this complication:
Urgent surgery The patient has heart or lung problems. The patient is on long-term use of opiates or tranquilizers or cocaine. The patient uses alcohol every day. 4.2. Complications from Intubation There are a number of complications associated with intubation manipulation such as:
Tooth trauma Injury to the throat or trachea Excessive accumulation of fluid in organs or tissues Bleeding Pulmonary Complications Gastrointestinal Reflux into the Lungs Physicians need to assess the patient's condition prior to the procedure to minimize the risk of possible complications. Simultaneously throughout the intubation process, the patient will also be carefully monitored.
To register for examination and treatment at Vinmec International General Hospital, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.