This is an automatically translated article.
The article was professionally consulted by MSc Vu Van Quan - Department of General Surgery & Anesthesia - Vinmec Hai Phong International General Hospital.Biliary stenting is a highly advanced technique used to treat bile duct obstruction. This method uses a synthetic plastic or metal stent, inserted into the bile duct to reduce the narrowing of the bile ducts.
1. What is biliary atresia?
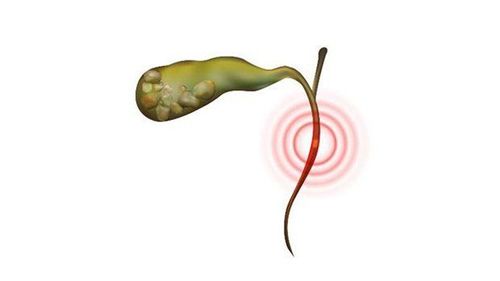
Bile is a fluid produced by the liver that helps the body digest fats. Bile is excreted through the bile ducts (bile ducts) and stored in the gallbladder. Bile secretion is regulated by a sphincter (sphincter) called the muscle of Oddi located at the junction between the common bile duct and the small intestine (duodenum). Biliary obstruction occurs when the bile duct that carries bile from the liver to the small intestine (duodenum) is blocked. Bile will be trapped in the liver because it cannot flow normally (called biliary obstruction). As a result, the patient has jaundice and cirrhosis because liver cells are destroyed, replaced by scar tissue. Scarring in the liver will impede blood flow through the liver, damaging liver cells and creating more scarring. In addition, obstruction of the bile duct also leads to digestive disorders, detoxification function, damage to organs adjacent to the liver, seriously affecting the patient's health.The main causes of biliary stricture include pancreatic cancer, gallbladder cancer, liver cancer, colon cancer, biliary tract injury during cholecystectomy, pancreatitis, primary sclerosing cholangitis, gallstones, abdominal trauma and complications after radiation therapy,...
2. What is biliary stenting?
Biliary stenosis leads to bile duct obstruction, dangerous to the patient's health. Therefore, patients with bile duct obstruction are often indicated for biliary stenting to drain bile out or into the duodenum.
Drainage of bile out is a simple procedure, low cost, but has the disadvantage of losing bile, affecting the quality of life of the patient because there is a tube that drains bile out of the body. And draining bile into the duodenum is a superior method, which can avoid the above disadvantages. Therefore, the method of internal bile drainage is being widely applied today. A biliary stent is a small, thin tube that is used to support the constricted portion of the bile duct. Stent tubes are made of synthetic resin or metal. Placement of metal-supported stents is shaped like a metal cage, has self-expanding features, has a relatively small diameter when passing through the skin, but when released into the biliary tract, it will expand to have a larger internal diameter. can reach 10mm. Self-expanding metal brackets are available in two types, uncovered and covered (the holes of the metal cage are sealed by a PTFE membrane surrounding the lumen of the stent). The covered type provides a longer stent transit time, but has the disadvantages of higher cost, larger diameter of the percutaneous passage, and the inability of the stent lumen to communicate with the bile ducts that drain into the covered stent area.
3. Biliary stenting methods to treat bile duct obstruction
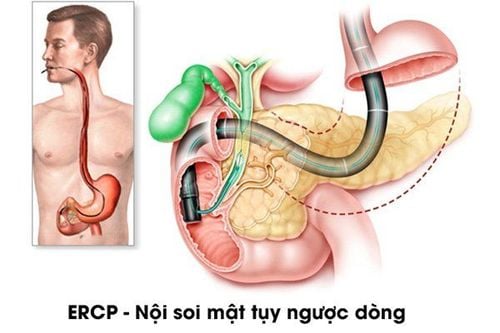
3.1 Endoscopic retrograde cholangiopancreatography
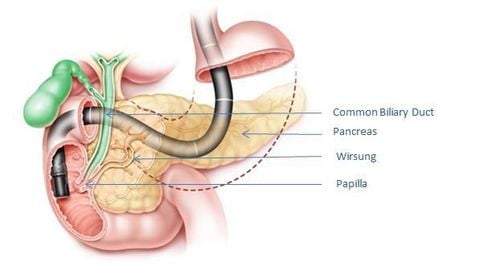
Endoscopic retrograde cholangiopancreatography (ERCP) is an endoscopic retrograde cholangiopancreatography - ERCP. This is an imaging technique used in the diagnosis of diseases of the liver, pancreas, gallbladder and biliary tract. Not only that, this technique also has the advantage of a therapeutic tool.
When performed, the endoscope will be passed through the patient's mouth, down the esophagus, through the stomach, duodenum and to the location where bile empties into the duodenum. In this position, a small tube is threaded through the endoscope to inject contrast material into the biliary tract. X-ray images will be taken as the contrast material moves through the bile ducts.
If the X-ray image shows a narrowing of the common bile duct, a stent will be placed in the bile duct to resolve the obstruction. To do this, special instruments will be threaded through the endoscope, cutting the sphincter (Oddi muscle) to access the biliary tree. In some cases, the doctor will first dilate the narrowed bile duct with a thin, elastic tube, then expand it with a balloon, and finally place a stent in the bile duct.
Chụp mật tụy ngược dòng qua nội soi (ERCP)
3.2 Percutaneous transhepatic cholangiography
The method of percutaneous transhepatic cholangiography is percutaneous transhepatic cholangiography - PTC. This technique is also used to diagnose and treat a blockage in the flow of bile from the liver to the small intestine. This procedure is often indicated in cases where endoscopic retrograde cholangiopancreatography has failed.
During the procedure, the doctor will use a fine needle, inject contrast dye through the skin into the liver or gallbladder, and take X-rays as the contrast moves through the bile ducts. When the location of biliary stricture is obvious, the doctor will place a stent in this position. Next, the doctor places a hollow needle into the biliary tree, threading a thin guide wire into the needle, toward the site of the blockage. The stent will be pushed forward along the wire and placed in place of the blockage in the bile duct.
4. How to perform biliary stenting procedure
4.1 Preparation The patient should fast for at least 6 hours prior to biliary stenting to ensure that the stomach and duodenum are clean and free of food; Patients fully informed about the drugs they are using to the treating doctor; The patient has no history of allergy to the iodine in the contrast medium; Take antibiotics before the procedure and continue for a few days afterward. 4.2 Perform ultrasound-guided percutaneous cholangiography; Placement of interventional access, usually use type 5F; Under the guidance of a screen (or a DSA angiogram) the wire is passed through the foramen into the duodenum. This is a crucial step to the success of the procedure. The performing physician needs to combine the hydrophilic guide wire and the catheter commonly used in angiography to pass through the obstructed site; After the catheter used in angiography passed through the site of obstruction and entered the duodenum, the doctor replaced the hydrophilic lead with an Amplatz rigid wire, changing the intervention path in accordance with the requirements of the stent (specifically, with If the covered stent is 10mm in diameter, the access route may have to be a 10F). The stent will be inserted through the patient's skin, following the Amplatz rigid wire through the narrow area. The length of the stent should be greater than the site of the fatigue duct stenosis but should not be too long because it may cause obstruction of the lateral biliary branches. In the case of using a covered stent, it is necessary to select the appropriate size for the lesion; Set the path to save the secret out to monitor and ensure safety. The drain is removed after 24 hours if there are no bleeding complications and good bile flow into the duodenum. 4.3 Post-treatment care Patients should be closely monitored for their health status to promptly detect complications; After performing endoscopic retrograde cholangiopancreatography, the patient will stay in the hospital until he is completely awake from anesthesia and has no complications; After percutaneous transhepatic cholangiography, the patient should lie on his right side for a minimum of 6 hours to reduce the risk of bleeding at the intervention site; Patients should be examined regularly to ensure the stent is working properly, early detection of recurrent symptoms of biliary stricture: change in color of stool and urine, itchy skin, jaundice, abnormalities in functional tests liver function,...
5. Value of biliary stenting in the treatment of bile duct obstruction
This treatment procedure relieves bile duct obstruction, helping bile flow better in about 94% of patients performed; It is a minimally invasive method, an effective and safe treatment, with little damage because it has little impact on the patient's body; Few complications; The postoperative period is short, the patient can eat, drink and walk right after, recover soon and be discharged from the hospital. Biliary stenting in the treatment of bile duct obstruction is a difficult technique, requiring a doctor with experience and skill. Therefore, if you want to choose this treatment method, you should do it at reputable hospitals.
Master. Doctor. Vu Van Quan has more than 10 years of experience working in the field of General Gastroenterology, specializing in examining and treating surgical pathologies of the gastrointestinal tract, liver, bile, pancreas and diseases of the abdominal peritoneum and abdominal wall.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.