This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Thuc Vy - Doctor of Diagnostic Imaging - Department of Diagnostic Imaging - Vinmec Nha Trang International General Hospital.Thymic tumors are much rarer than other cancers, with the 5-year survival rate for people with thymoma being 71% if diagnosed and treated early. Therefore, the diagnosis of thymoma plays an important role and needs to be clearly understood.
1. What is a thymus tumor?
Thymus cancer and thymic carcinoma are also known as thymic epithelial tumors (TETs) because these tumors start in thymic epithelial cells. These are two rare cancers that can form in the cells that cover the outer surface of the thymus. Previously, thymoma was divided into benign thymoma and malignant thymoma based on the growth of the tumor. However, now most thymomas can become cancerous over time. The World Health Organization (WHO) classifies thymoma into the following categories:
● Type A: The cells in these tumors are spindle-shaped or oval-shaped epithelial cells that look fairly normal. This is the rarest type of thymoma, but it seems to have the best prognosis. Nearly 100% of people with this type of tumor live at least 15 years after diagnosis.
● Type AB: also known as mixed thymoma. This type is the same as type A but there are also areas of mixed lymphocytes within the tumor. The chances of recovery for people with this disease are also very good. About 90% of patients can live at least 15 years after diagnosis.
Tế bào lympho quá nhiều gây ra u tuyến ức loại B1
Type B1: also known as lymphocyte-rich thymoma and its structure is very similar to the normal structure of the thymus. This type of thymoma has many lymphocytes in the tumor. The chances of recovery for people with type B1 thymoma are also very good. About 90% of people can live at least 20 years after diagnosis.
Type B2: This type also has a lot of lymphocytes, but the thymus epithelial cells are larger with abnormal cell nuclei (the part of the cell that contains the DNA). About 60% of people with this condition live for at least 20 years after diagnosis.
● Type B3: Also known as epithelial thymoma, atypical thymoma, squamous thymoma, and differentiated thymic carcinoma. This type has few lymphocytes and the thymus cells look abnormal. About 40% of people with the disease live at least 20 years after diagnosis.
● Type C: This is the most dangerous type also known as thymic carcinoma. It contains cells that look like abnormal cells under a microscope. The cells may no longer look like thymus cells. These tumors often grow into nearby tissues or spread to other distant tissues and organs (metastasize) at the time they are found. This type of thymoma has the worst prognosis. About 30% of people with the disease live at least 5 years after diagnosis.
Type AB and type B2 are the two most common types of thymoma. Type A is not common. The outlook for survival from category A to type C tends to be dire. However, for most types of thymoma, stage (the extent of growth and spread) is a better predictor of treatment outcome for the person with the disease.
2. How many stages of thymus tumor?
Thymoma is divided into 4 stages:
● Stage 1: This stage is only found in the thymus. All cancer cells are located in the cystic sac surrounding the thymus.
● Stage 2: The tumor has spread through the cyst and into the fat around the thymus or into the lining of the chest cavity.
● Stage 3: The tumor has spread to nearby organs in the chest including the lungs, the sac around the heart, or the large blood vessels that carry blood to the heart.
● Stage 4: Stage is divided into two subtypes IVA and IVB (depending on where the cancer has spread). IVA - cancer has spread throughout the lungs or heart. IVB - cancer has spread to the blood or lymphatic system.
In addition, the TNM (tumor size-tumor-site-metastasis) tool can be used to stage thymoma. There are 5 stages which are 0 and I to IV.
2.1. Tumor size (T)
● T0: No evidence of primary tumor
● T1: Tumor is only in the thymus or has grown into nearby fatty tissue. T1a-The tumor has spread to the fatty layer surrounding the thymus. T1b-tumor that has grown into the lining of the lung next to the tumor (mediastinal pleura).
● T2: The tumor has grown into nearby fatty tissue and into the sac around the heart (pericardium).
● T3: The tumor has spread to nearby tissues or organs including the lungs, the blood vessels that carry blood in or out of the lungs, or the nerves that control breathing.
● T4: The tumor has spread to nearby tissues or organs including the trachea, esophagus, or blood vessels that pump blood away from the heart.

Khối u lan đến các cơ quan lân cận (Hình ảnh minh họa)
2.2. Tumor location (N)
● N0: Tumor has spread into lymph nodes
● N1: Tumor may have spread to nearby lymph nodes
● N2: Tumor has spread to lymph nodes deep in the chest cavity or neck
2.3. Metastasis (M)
● M0: The tumor has not metastasized
● M1: The tumor has spread to organs near the thymus, such as the lungs and blood vessels. M1a-The tumor has spread to the lining of the lungs (pleura) or the pericardium (pericardium). M1b-tumor may have spread to the heart.
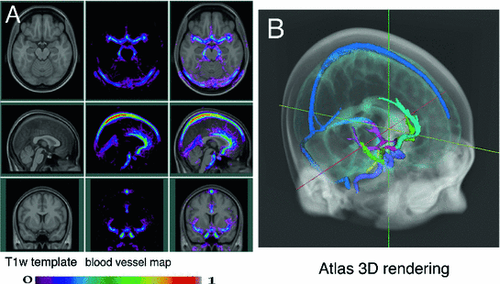
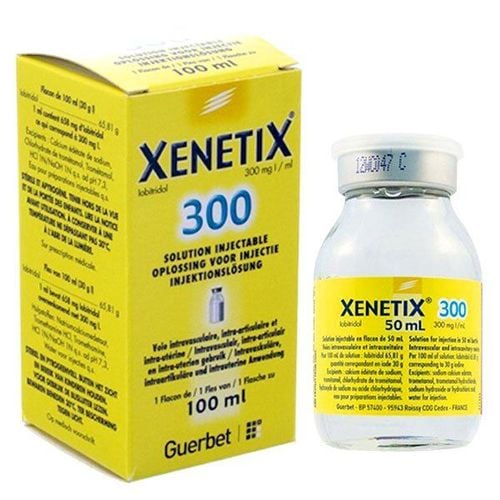
3. X-ray methods to diagnose thymoma
Chest X-ray: Using an energy beam that can pass through the body onto a film to create an image of the internal body area, this technique has many limitations, can miss lesions and cannot be assessed in depth. Tumor stage assessment should no longer be used in practice for diagnosis and treatment. CT/CT scan: This technique creates a series of detailed images (3D images) of areas inside the body. The images are taken by a computer linked to a tomography machine that uses X-rays. Contrast drugs are injected intravenously or taken orally to help organs or tissues show up more clearly. In addition, this technique can be used to measure the size of the tumor and assess the stage of TNM disease. This is the most appropriate and most widely chosen technique in practice for the diagnosis of thymic tumors. MRI scan: This procedure uses a magnetic field, radio waves, and a computer to create a series of detailed pictures of areas inside the body such as the chest. In addition, this procedure requires the use of more contrast agent from the clearer image. The drug is injected into a vein. In addition, MRI can also measure tumor size. However, this technique has many limitations and has not been widely used. ● PET scan: This is a procedure to find melanoma cells in the body. Use a small amount of radioactive glucose injected into a vein. The PET scanner rotates around the body and creates a picture of where glucose is being used by tumor cells in the body. Melanoma cells will appear brighter in the image because they are more active and take up more glucose than normal cells.PET also helps doctors better know if a change seen on imaging tests is a tumor. For example, if you've been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to the lymph nodes or other parts of the body.

PET scan giúp kiểm tra tế bào u ác tính trong cơ thể
Thymus tumor is a rarer disease than other cancers, but when this disease is diagnosed and treated in time, the chance of survival is very high. Accordingly, thymoma can be diagnosed by X-ray, CT, MRI and PET imaging techniques. Therefore, when seeing signs of disease, patients should go to medical facilities for examination and treatment.
Currently, Vinmec International General Hospital has brought modern imaging techniques to serve the examination and treatment of patients. With a team of experienced and qualified medical doctors, we will bring optimal treatment results to customers.
To register for medical examination and treatment at Vinmec International General Hospital nationwide, customers can register for examination HERE for support.
Reference source: cancer.net