This is an automatically translated article.
Currently, the situation of bacteria resistant to antibiotics is increasing, this is an urgent problem, threatening the health of the whole community. Therefore, each citizen needs to improve their own knowledge to limit the increase of antibiotic-resistant bacteria. Let's find out together the answer to the question of how bacteria are resistant to antibiotics?1. Why are bacteria resistant to antibiotics?
Bacteria are very small living organisms, found everywhere around us, most bacteria are harmless, they even bring certain benefits. However, there are some bacteria that are harmful to plants, animals and humans. Antibiotics that kill or prevent the growth of bacteria should be used in the treatment of infections and diseases caused by bacteria, besides, some bacteria find ways to survive. and multiply.
Some bacteria are inherently resistant to certain antibiotics called natural resistance. For example, benzyl penicillin has very little effect on most organisms found in the human digestive system (intestines).
Some bacteria have developed resistance to antibiotics that were once commonly used to treat them called acquired resistance. For example, Staphylococcus aureus (also known as 'golden staph' or MRSA) and Neisseria gonorrhoeae (the cause of gonorrhea) are now almost always resistant to benzyl penicillin. In the past, these infections were usually controlled with penicillin.
MORE: Antibiotics and bacteria: What to know

Một số vi khuẩn có khả năng đề kháng lại thuốc kháng sinh
2. What are the types of antibiotic-resistant bacteria?
Antibiotic resistant bacteria have the following forms:
2.1 Counterfeit resistance
Pseudo-resistance is not of genetic origin but due to one of three factors or possibly a combination of two or even three antibiotic factors - patient - bacteria.
Due to antibiotics: Due to incorrect antibiotic selection to treat pathogens, inappropriate use in terms of dosage, route of administration, time between doses, or use of low-quality antibiotics good. Because of the patient: The immune system is not good or the antibiotic is limited to diffuse into the infection. Bacterial: Because bacteria are in a dormant state, they are not affected by antibiotics. For example, tubercle bacilli are located in the "caves" of tuberculosis.
Hệ miễn dịch của người bệnh không tốt gây ra hiện tượng đề kháng giả
2.2 Natural resistance
Natural resistance is true resistance due to some bacteria species that are not resistant to certain antibiotics. For example, penicillin G has no effect on Pseudomonas aeruginosa.
2.3 Resistance acquired
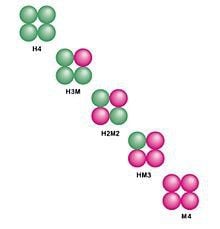
Acquired resistance is also a true type of resistance but is due to a genetic event of mutation or acquisition of a resistance gene, that is, being susceptible to antibiotic resistance. These genes may be located on one, several or all of the bacterial genetic elements, including chromosomes, plasmids, and transposons.
SEE ALSO: Antibiogram - solutions to reduce antibiotic resistance
3. Bacteria resistant to antibiotics by mechanism?
To survive, bacteria are resistant to antibiotics by very diverse mechanisms based on resistance genes, collectively known as resistance mechanisms, including:
3.1 Reduces drug permeability
Bacteria resistant to antibiotics by reducing the permeability of the drug wall or outer membrane and plasma membrane, so the antibiotic cannot penetrate the bacterial cell. Another way is to increase the activity of the pump system (efflux) to push the antibiotic out of the cell.

Làm giảm tính thấm thuốc là một cách khiến vi khuẩn kháng thuốc kháng sinh
3.2 Changing the target of impact
Target of action, also known as a receptor or drug-binding receptor, is the way a drug attaches to cause a bacteria-killing effect. Since then, bacteria are resistant to antibiotics by modifying drug-binding receptors, so the antibiotic cannot attach to the target to be effective. For example, bacteria are resistant to antibiotics by altering the ribosome, which is the binding site for antibiotics, streptomycin, and erythromycin.3.3 Altering metabolic pathways
With other organisms that attack the metabolic pathways of bacteria so that they cannot grow and multiply, bacteria become resistant to antibiotics by producing opposing enzymes called isoenzymes, which disrupt the antibiotic's affinity for bacteria. bacteria, making the drug ineffective.For example, sulphonamides, trimethoprim are bacteriostatic by blocking the synthesis of folic acid by bacteria. Bacteria produce isoenzymes that counteract the effects of antibiotics.
Vi khuẩn tạo ra isoenzyme làm giảm đi tác dụng của thuốc kháng sinh
3.4 Generating enzymes to change the molecular structure of antibiotics
Some bacteria are resistant to antibiotics by creating enzymes to change the molecular structure of antibiotics, thereby breaking down or inactivating the effect of the drug. For example, bacteria secrete Ophosphotransferases, N-acetyltransferases that modify aminoglycoside antibiotic molecules or secrete beta-lactamase enzymes that inactivate beta-lactam antibiotics.Usually, an antibiotic-resistant bacteria is not caused by a single mechanism mentioned above, but often combined with many different mechanisms at the same time. Besides, this antibiotic-resistant bacteria can cause resistance to other antibiotics of the same group or similar structure, called cross-resistance.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: .cdc.gov, who.int/













