This is an automatically translated article.
The article was professionally consulted by Pharmacist Duong Thanh Hai - Faculty of Pharmacy - Vinmec Times City International HospitalAntibiotics are a great man-made weapon against bacterial infections, but now bacteria are resistant to the antibiotics that are used to kill them. Antibiotic resistance is the biggest threat to the health sector in particular and society in general.
1. What is antibiotic resistance?
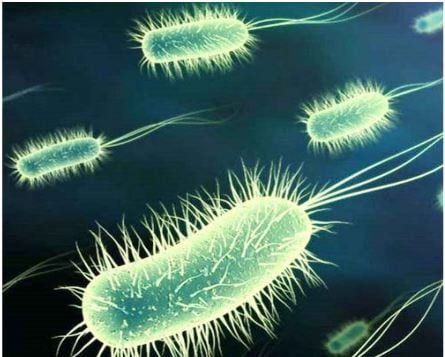
Antibiotic resistance does not mean that the body is resistant to the effects of antibiotics. Antibiotic resistance occurs when pathogens or bacteria have the ability to develop resistance to antibiotics, making them unable to kill or stop their growth.
Bacteria can be naturally resistant to antibiotics or develop resistance through genetic mutations or the acquisition of resistance genes from another species of bacteria.
Antibiotic-resistant bacteria make bacterial infections difficult, even impossible, to treat. Infections caused by resistant bacteria force doctors to use alternative antibiotics, which are often more toxic, leading to longer hospital stays and costly medical expenses.
No one can completely avoid the antibiotic resistance of bacteria, even advanced medical techniques such as cardiopulmonary support, dialysis, transplantation... also depend on the ability to fight. antibiotic-resistant bacteria.
Although mankind is making efforts to develop new antibiotics, antibiotic resistance continues to happen at a faster and more complex rate.

2. Current status of antibiotic resistance
Antibiotic resistance can affect anyone, not only the medical industry but also the veterinary and agricultural industries. The situation of antibiotic resistance in recent decades is a global threat, especially in developing countries with infectious diseases still accounting for a high proportion in the disease structure such as gastrointestinal infections. , respiratory tract, sexually transmitted diseases and nosocomial infections.... Control of these diseases has become more and more difficult due to the development and spread of antibiotic resistance in bacteria. According to statistics in the United States, more than 2 million people contract bacterial infections every year and at least 23,000 of them die.
Antibiotic-resistant bacteria that pose a threat to global health are being warned including: Carbapenem-resistant intestinal Gram-negative strains, vancomycin-resistant enterococci, methicillin-resistant Staphylococcus aureus, pneumococcal disease, and gonorrhea. drug resistance, Clostridioides difficle, drug-resistant tuberculosis... Antibiotic resistance is a great threat because pathogenic bacteria are no longer afraid of human weapons. At this time, antibiotics only inhibit or kill beneficial bacteria, while resistant bacteria will multiply rapidly, spread and cause uncontrollable infections.
So, how can bacteria become resistant to antibiotics?
First: bacteria prevent antibiotics from getting inside them by strengthening or modifying the structure of their protective membranes. For example, Gram-negative bacteria have an outer membrane to prevent antibiotics from penetrating inside.
Second : bacteria create pusher pumps to pump antibiotics out. For example, blue pus bacillus can produce a pump that pushes the group of quinolones and beta lactams, leading to inactivation of antibiotics.
Third: bacteria produce enzymes (enzymes) to destroy antibiotics such as penicillinase, broad-spectrum beta lactamase, carbapenemase... This is a common way that bacteria produce to fight most pathogens. antibiotic group. For example, Klebsiella pneumoniae produces carbapenemase enzyme KPC destroys carbapenem group; Escherichia coli produces broad-spectrum beta lactamase ESBL resistant to cephalosporins...
Fourth: bacteria change the structure of their parts, making antibiotics unrecognizable. For example, altering the penicillin-binding protein PBP is how bacteria resist beta-lactam antibiotics. Mutations in the gene that codes for DNA-gyrase are the way to resistance to the quinolone class of antibiotics.
3. Limiting antibiotic resistance
Antibiotic resistance is increasing mainly due to overuse of antibiotics, misuse of antibiotics and poorly implemented infection prevention measures.
To prevent antibiotic resistance from becoming more serious, the following principles should be well followed:
Antibiotics only work on bacteria, not helping to treat viral diseases such as flu, common cold often. Use antibiotics only when absolutely necessary and must be prescribed by a doctor. Even if the disease is cured, do not stop taking the medicine until the end of the period prescribed by your doctor. Do not arbitrarily buy antibiotics or ask your doctor to prescribe antibiotics without prescription. Each antibiotic only works on certain types of bacteria, it is necessary to use antibiotics suitable for the strain of bacteria causing the disease. Do not share antibiotics with relatives or friends. Prevent bacterial infections by regularly washing hands, eating clean, avoiding close contact with sick people and being fully vaccinated.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














