This is an automatically translated article.
The article is professionally consulted by Master, Doctor Phan Ngoc Hai - Department of Pediatrics - Neonatology - Vinmec Danang International General HospitalHepatitis B in young children is a big obsession for parents. Because hepatitis B is one of the extremely dangerous diseases, caused by the hepatitis B virus. Hepatitis B in children is clinically different from that of adults, and the treatment of chronic hepatitis B in children is also much more complicated. Therefore, parents should equip themselves with the necessary knowledge to be able to protect the health of their babies in the safest and most effective way.
1. Causes of Hepatitis B in Children
Hepatitis B is an infectious disease caused by the hepatitis B virus. The disease is transmitted through 3 ways: blood, sexual and mother-to-child transmission.The cause of hepatitis B infection in young children is mainly due to the disease transmitted from mother to child. In fact, in Asian countries, this is a common route of hepatitis B infection because people's knowledge about this disease is limited, many people are not fully vaccinated. In Vietnam, too, many women are not screened before and during pregnancy. According to some studies, in Vietnam, more than 10% of pregnant women are infected with hepatitis B virus. This is a very large percentage.
If the mother is infected with hepatitis B in the early stages of pregnancy (the first 3 months), the mother has a low rate of transmitting viral pathogens to the baby (about 1%) and if the mother has hepatitis B in the second 3 months of pregnancy, the rate of mother transmitting pathogens to her baby is up to 10%, especially if the mother is sick in the last 3 months of pregnancy, the rate of mother passing the pathogen to her baby is up to 10%. up to 60-70%. Thus, the rate of pregnant mothers infected with hepatitis B virus passing to the fetus from the 3rd month onwards is very high.
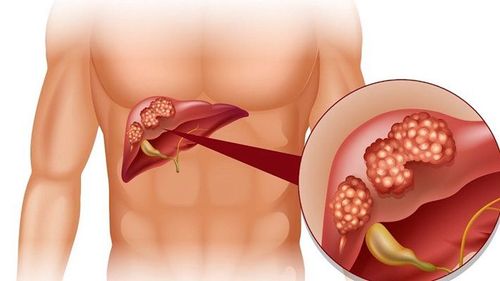
About 90% of children are infected during infancy. The cause is the virus in the blood, the mother's fluids will be transferred to the baby's body. Especially babies with immature immune systems will not have enough resistance to destroy the virus. From there, the disease will easily develop and turn into a dangerous chronic stage, with no cure. Newborns with hepatitis B are at high risk of complications from cirrhosis and liver cancer in adulthood.
Today, to assess the progression of hepatitis B virus in the infected person's body, there are many different methods, but common and can be applied in laboratories of provincial hospitals is to determine HBsAg and HBeAg.
HBsAg is the surface antigen of the hepatitis B virus, when the test is positive, it means that the person's body has been infected with this virus. HBeAg is also an antigen of this virus (core antigen). When this antigen appears and exists, it shows that the virus is multiplying (proliferating and liver cells are being invaded). During this period, if the liver enzymes are tested (SGOT, SGPT, GGt), these liver enzymes are found to be very high (at least twice the normal value) due to the destruction of liver cells by the virus. release liver enzymes. Statistics show that, when a pregnant woman's blood test in the third trimester shows both HBsAg and HBeAg positive, the mother-to-child transmission rate is up to 90-100%. However, if only HBsAg is positive, while HBeAg is negative, the rate of mother-to-child transmission is much lower (about 20%).

2. Symptoms
When infected with hepatitis B virus, children can carry the virus without showing any symptoms and still live, study and develop normally. When there are certain favorable conditions such as severe infection, poor health..., the virus will cause acute hepatitis episodes.In the period before jaundice, usually lasts 7-10 days with flu-like symptoms such as fever, runny nose, fatigue, loss of appetite, nausea, possibly diarrhea, constipation, bloating, In breastfed babies stools may be pale. The liver may be enlarged, painful, right lower quadrant, dark urine. At that time, parents need to immediately take the child to a hospital or a liver specialist clinic for early appropriate treatment.
Followed by a period of yellow skin, dark urine, yellow eye mucosa. There may be spots, hemorrhagic patches on the skin due to impaired liver function. Often the liver is enlarged, painful, pain in the right lower quadrant in older children, may have an enlarged spleen (however, if the liver size is small, the prognosis is bad). The child's abdomen may be slightly distended, eat poorly, and have mucus-like stools. At this stage, the child's fever subsides, the jaundice gradually decreases and disappears within 2-3 weeks from the onset of the disease. The above symptoms gradually decrease, the child eats better, the urine is clear.
In infants, the manifestations of the disease may not be obvious, sometimes only jaundice, poor feeding. Mothers often think that it is physiological jaundice, or do not pay attention because the child is always kept in a dark room, so they do not take the child to the doctor and treat in time, causing serious consequences such as liver failure, cerebral blood...
When hepatitis B infection with surface antigen (HbsAg) remains in the patient's blood for more than 6 months, it is considered chronic, it is characterized by 4 immune stages of the disease.
Stage 1: HBsAg and HBeAg detected HBV DNA > 100,000 copies/ml.
Liver enzymes (ALT, AST) are within normal limits.
No signs of hepatitis and cirrhosis or very mild.
Stage 2: HBsAg and HBeAg still have HBV DNA > 100,000 copies/ml.
Liver enzymes (ALT, AST) increase continuously.
Possible progression of hepatitis and cirrhosis.
Stage 3: HBsAg is still present HBeAg disappears, anti-Hbe appears.
HBV DNA < 10,000 copies/ml or undetectable.
Liver enzymes (ALT, AST) normal.
No signs of hepatitis, signs of cirrhosis will go away.
Stage 4: HBsAg is still present HBeAg is still negative and anti-Hbe is still positive.
HBV DNA > 10,000 copies/ml.
Liver enzymes (ALT, AST) normal or elevated.
Hepatitis can attack and potentially lead to cirrhosis.
3. Treatment

In addition, a complete panel of liver function and platelets should be checked periodically. An increased ratio of AST to ALT is often a sign of increasing fibrosis, especially if the AST is greater than the ALT.
The possibility that a child with chronic hepatitis B infection with AST > ALT is at risk for cirrhosis is significant and to support this assessment a liver biopsy may be warranted. However, AST > ALT may also be transiently seen in children who have recently consumed alcohol or after vigorous physical activity, and other possibilities need to be ruled out before performing a search for fibers. progression due to HBV. Thrombocytopenia may be an early sign of portal hypertension in the setting of cirrhosis.
An increase in serum liver enzymes (ALT) indicates the degree of hepatocellular necrosis, i.e. liver damage. In adults, the upper limit of normal for ALT is >30 IU/L for men and >19 IU/L for women. However, the ULN in children has not been established, and for children, the ULN used often varies by laboratories and the age of the child. In the absence of pediatric criteria, ALT elevations should be considered greater than laboratory ULNs or > 40 IU/L.
3.2 Children with normal ALT In the treatment of children with chronic hepatitis B infection, identifying those who do not need treatment is just as important as identifying those who do.
As noted above, the majority of children with perinatal hepatitis B infection remain in stage 1 throughout childhood and often into adulthood. The longest duration of this phase is commonly seen in individuals infected with HBV genotype C (HBV has 8 genotypes A to H) and the rate of HBeAg seroconversion in children infected with HBV genotype C is very low. These children are consistently HBeAg positive with HBV DNA as high as 100,000 copies/ml and possibly higher. However, there was no disease-causing immune response activity and ALT remained in the normal range. Published clinical data supporting the treatment of children during this period is very limited.
3.3 Children with persistently elevated ALT liver enzymes Persistently high serum ALT levels are characteristic in stage 2 of the disease.
Elevated serum ALT level is an indicator of hepatocellular necrosis. Specifically, if a child has a serum ALT level greater than 1.5 times the laboratory ULN or greater than 60 IU/L (ie, 1.5 x 40 IU/L), these children should be further evaluated for serum ALT levels. HBV DNA and liver histology to consider appropriate treatment.
If serum ALT level is lower than above, follow up more than 2 times for at least 6 months for HBeAg positive patients and more than 3 times for at least 12 months for HBeAg negative patients .
The reason for continuous high serum ALT monitoring for at least 6 months in HBeAg-positive patients is to avoid treating a child during spontaneous HBeAg seroconversion and the disease improves without need treatment.
3.4 The following special cases require long-term treatment Rapidly decline in liver function. Cirrhosis (compensated or decompensated). Glomerulonephritis caused by HBV infection. Recurrent hepatitis B virus infection after liver transplantation. Presence of viral strains (HBV/HIV, HBV/HCV, HBV/HDV). Children with a family history of hepatocellular carcinoma. Pregnant women have a high viral load (> 20,000,000 IU/ml) during the third trimester.

4. Prevention
When the baby is born, if the mother is found to be positive for hepatitis B, the baby will be vaccinated with hepatitis B vaccine and antisera to help protect the baby in the postpartum process. Children should be fully vaccinated against hepatitis B and have antibody titers checked when eligible. Most of the above will help the baby prevent effectivelyVaccination is the most effective and guaranteed way of prevention. Babies born to mothers with hepatitis B should be given one shot of anti-HBV globulin and one dose of hepatitis B vaccine within the first 12 hours after birth. Then, inject the full dose according to the regimen, when the child is 1 month old, get the 2nd injection, 2 months old get the 3rd dose and repeat at 12 months old.
If the child is diagnosed with the disease, it is necessary to follow the instructions and advice of the doctor because hepatitis B in children is easy to develop into a chronic one. Along with that is to take the children to the doctor periodically to check their health and monitor the disease situation.
At Vinmec International General Hospital, the vaccination process is carried out carefully, in accordance with the requirements of the Ministry of Health. Children will be screened before vaccination and health monitoring after vaccination. Vaccines at Vinmec are imported from famous big companies in the world, have clear inspection, are preserved by Vinmec on a modern cold chain in accordance with the instructions of the Ministry of Health and the World Health Organization. gender.
Parents can consult information about immunization vaccines, including hepatitis B vaccine at Vinmec International General Hospital. Customers can directly go to Vinmec health system nationwide to visit or contact the hotline here for support.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.