This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Helicobacter pylori is the main cause of stomach diseases. Recently, researchers have demonstrated a potential role for Helicobacter pylori (H. pylori) infection in the initiation, development, or persistence of atherosclerosis and coronary heart disease.
Abbreviation
Macrophages (abbreviated as M)
Coronary heart disease (CHD)
Helicobacter pylori (H. pylori)
Bacterial lipopolysaccharide – lipopolysaccharide factor (LPS
)
1. An overview of Helicobacter pylori (H. pylori) bacteria
This gram-negative bacterium was described by Marshall and Warren in 1984. The majority of subjects infected with H. pylori carry and transmit no symptoms. However, in some people, these bacteria can cause peptic ulcers and even stomach cancer. The prevalence of H. pylori infections and the fact that they are often asymptomatic may suggest that, similar to the gut microbiome, H. pylori may provide antigens that not only stimulate a response local but also systemic inflammation.
Many authors have discussed the findings and underlying concepts of the potential role of Helicobacter pylori (H. pylori) infection in the initiation, development, or persistence of atherosclerosis and vascular disease. coronary (coronary artery disease). Recently, a possible link between H. pylori infection and extragastric disorders has been suggested. Knowledge of the etiology of atherosclerosis together with current findings in the field of H. pylori infection form the basis for the newly proposed hypothesis that the two processes may be related. Many studies confirm an indirect association between the prevalence of H. pylori and the occurrence of coronary heart disease. According to the majority of findings, H. pylori's involvement in this process is based on chronic inflammation that may facilitate coronary artery disease-associated pathologies. It needs to be elucidated, if the infection initiates or only accelerates the formation of atherosclerotic plaques.

2. The pathogenicity of Helicobacter pylori
Helicobacter pylori (H. pylori) is a Gram-negative spiral bacterium that lives on the gastric mucosa of nearly half of the human population. A characteristic feature of H. pylori infection is an exaggerated inflammatory response. The majority of H. pylori infections remain asymptomatic. However, it still leads to the development of histological gastritis with the recruitment of immune cells. Approximately 10% of infected subjects develop symptomatic gastritis, erosive or peptic ulcer. Stomach cancer is the most severe consequence of H. pylori infection. Recently, the possible link between chronic H. pylori infection and extra-gastric disorders - including cardiovascular disease has been well studied. Many recent studies confirm or exclude possible associations between chronic bacterial infections and the occurrence of coronary heart disease in different populations, especially in the context of H. pylori.
Given the importance of the studies performed, it is likely that H. pylori infection is involved in the development of coronary heart disease, however, much work remains to be done to clarify whether the relationship is clear. whether this association is direct (with the involvement of H. pylori antigens and antibodies) or indirect (with the involvement of molecules implicated in progressive inflammation/or initiation of coronary disease) .
3. Scientists are clarifying the role of Helicobacter pylori in coronary heart disease
Since classical risk factors do not explain all cases of coronary heart disease, the notion that atherosclerotic disease may have an infectious background should be considered. The role of pathogenic viruses and bacteria including Helicobacter pylori is now considered to be factors involved in the development of coronary heart disease. Chronic infections may influence the course of coronary artery disease through various mechanisms such as chronic inflammatory responses, autoimmune processes, and modification of classical coronary disease risk factors. The pioneering finding of Mendall et al., published in 1994, showed that patients with coronary artery disease had elevated serum levels of anti-H.pylori antibodies. Following this finding, some authors confirmed and some ruled out the existence of this connection. Currently, there is no consensus on the role of H. pylori in the etiology or progression of coronary artery disease. To characterize the involvement of H. pylori in the development of coronary heart disease, it is necessary to find the largest number of studies that reliably confirm this relationship.
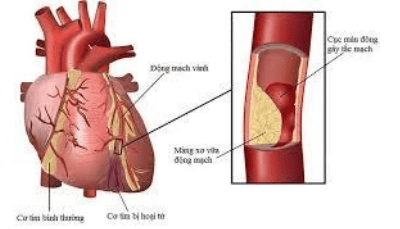
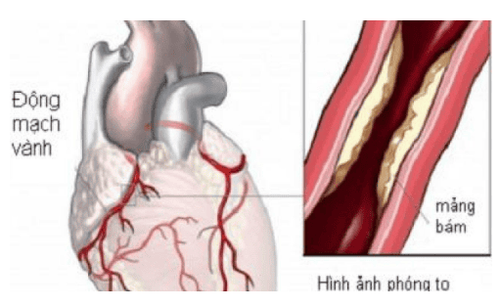
4. Pathophysiology of coronary artery disease
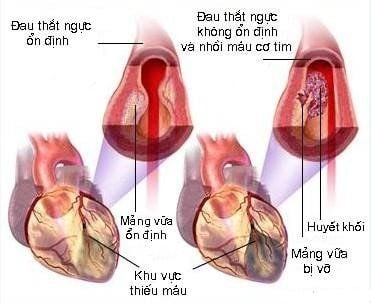
Coronary heart disease is one of the most serious chronic diseases of the coronary arteries - an important health and social problem that is often life-threatening. It occurs as a result of endothelial dysfunction within the vessels, accompanied by elevated blood pressure, vascular remodeling, local inflammation, platelet aggregation, and coagulation. These disorders promote the formation of atherosclerotic plaques, which often become unstable and subsequently rupture. This can reduce blood flow leading to a blood vessel blockage or a heart attack. Classic risk factors for coronary heart disease include smoking, hypertension, increased levels of total cholesterol, triglycerides, and low-density lipoprotein (LDL) compared with decreased fraction of high-density lipoprotein (HDL). , diabetes mellitus, as well as increased homocysteine and clotting factors. Factors that tend to increase the likelihood of developing coronary heart disease are obesity, physical inactivity, prior history of coronary heart disease in a relative, male gender, low socioeconomic status, as well as demographic factors. ethnicity and behavior.
5. Role of LDL cholesterol and phagocytic colon in coronary artery disease
Coronary heart disease is a group of symptoms caused by chronic malnutrition and hypoxia of myocardial cells, accompanied by inhibition, burning, feeling of burden, discomfort and chest tightness. These disorders are histologically a consequence of atherosclerosis characterized by the accumulation of macrophages (abbreviated as MØ), LDL fractions, macrophage-derived foam cells Cells are filled with a complex of oxidized LDL cholesterol and extracellular (ox) deposited in the vessel. On the inner surface of the vessel, lipid deposits are formed, which are gradually enclosed by a connective tissue and undergo fibrosis. According to statistics of the World Health Organization (WHO), ischemia related to atherosclerotic plaque is the main cause of coronary heart disease, 70% of heart failure cases and 80% of sudden cardiac death. . The natural history of atherosclerosis suggests that lesions in the arteries may have occurred in utero or during childhood. However, the clinical manifestations of atherosclerosis are related to the presence of atherosclerotic plaques, which usually develop after the age of 50 in men and in women after menopause.
6. Vascular endothelial dysfunction as an initiating factor of atherosclerotic plaque formation
The inside of the blood vessel is covered by an adjacent layer of endothelial cells (0.2-0.3 mm in size) attached to the basement membrane and extracellular matrix molecules via seamless adhesion molecules . The endothelium is in contact with smooth muscle cells through openings and is permeable to electric currents, ions, and low molecular weight compounds. The human vascular endothelium is a barrier that separates blood containing clotting proteins, platelets, and inflammatory cells, from the connective tissue and muscular layers of the blood vessel walls. The balance between the internal and external environment of the vessel depends on the mechanical, chemical and immunological reactions occurring in the endothelial cell.
The endothelium is affected by the physical pressure of the blood stream (hemodynamic force), various solutes, and immune cells. The endothelium provides many substances that act as angiogenic and vasoconstrictive factors (which determine the proper tension of the vessel wall), cytokines, and adhesion molecules (responsible for interacting with blood cells and development of an inflammatory response), factors involved in coagulation and fibrinolysis. All together, the endothelium plays a role in maintaining vascular homeostasis as determined by its bulk, distribution, and ability to receive and respond to signals from the external environment (stimulation). hemodynamic and chemical, pO2), by altering the expression of active substances and proteins.
7. Role of adhesion molecules in coronary artery disease
The endothelium exhibits structures required for adhesion, migration, activation and diapedesis of immune cells and platelets, allowing the development of an inflammatory response. These are mainly adhesion molecules (selectins) such as: P-selectin (platelets), E-selectin (endothelial) and L-selectin (leukocytes) and immunoglobulin-derived adressins, including : intracellular adhesion molecules (ICAM) -1 and -2, vascular cell adhesion molecule 1 (VCAM-1), platelet endothelial cell adhesion molecule 1, and macrophage chemotactic protein cell-1 (MCP-1).
If the endothelium is damaged, it loses its functional integrity and homeostasis, leading to the appearance of multiple lesions. This dysfunction often leads to increased tension, vascular remodeling, wall inflammation, and increased adhesion and platelet aggregation. These processes contribute to the development of atherosclerosis or the instability of existing atherosclerotic plaques.
8. Coronary artery disease as an inflammatory process
In the late 1990s, many authors believed that the atherosclerotic process was a response to mechanical trauma, leading to loss of the endothelial cell layer in the vessels. Since the majority of coronary artery disease symptoms are caused by local and systemic inflammatory responses, recent focus has been on the role of inflammation in the development of atherosclerosis. Inflammatory markers, such as C-reactive protein (CRP) were found to be higher in coronary heart disease patients compared with controls, similar to levels of interleukin (IL)-6 and mass necrosis factor Tumor alpha (TNF-α) in plasma and supernatant of immune cells were stimulated in vitro with bacterial lipopolysaccharide (LPS). However, it is clear that endothelial dysfunction and elevated cholesterol play an important role in inflammation. Cholesterol contributes to the localization of atherosclerotic lesions, preferentially at sites leading to activation of the endothelial NF-κB signaling pathway. The inflammatory response is characterized by the influx of MØ and monocytes to the endothelium, with the latter being transformed first into MØ and then foaming cells prior to ingestion of oxLDL.
9. The role of inflammatory factors
The protein components of LDL particles are processed by macrophages and dendritic cells and presented to T cells in the context of activated class II MØ major histocompatibility complex and other inflammatory cells chemokine release stimulates migration of smooth muscle cells which, together with foam cells, form a fibrous cap. This process is facilitated by interferon gamma (IFN-γ) and TNF-α secreted by T helper (Th)-1 lymphocytes, as well as by IL-12 produced by macrophages and cells foam. It then undergoes apoptosis and together with cholesterol crystals forms a lipid coating. It has been revealed that atherosclerotic lesions are associated with increased reactivity of immune cells. Wounded tissues secrete IL-33 to alert the immune system, induce expression of adhesion molecules, and attract Th2 lymphocytes that deliver the anti-inflammatory cytokine IL-4. However, increasing evidence indicates that IL-4 may play a role in atherosclerosis through induction of inflammatory responses, such as upregulation of VCAM-1 and MCP-1.10.The role of inflammatory factors in the vascular endothelium
The first group includes surface lectins while CagA, VacA and LPS represent the second group. H. pylori LPS shares a number of features in common with human tissues. These are the Lewis (Le) determinants: LeX, LeY, LeXY are present in the specific O chain of H. pylori LPS and on the surface of host cells: red blood cells, granulocytes, monocytes, cells epithelial cells and vascular endothelium. Therefore, H. pylori may reduce its recognition by host immune cells and pose a risk of autoantibody production. H. pylori LPS of the LeXY type attenuated the phagocytic activity of granulocytes, the cytotoxic activity of NK cells and the proliferation of lymphocytes. It binds to the non-integral dendritic cell-specific intercellular adhesion molecule-3 (DC-SIGN) and may interfere with the development of a specific immune response.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
1. Libby P, Theroux P. Pathophysiology of coronary artery disease. Circulation . 2005;111:3481-3488. [PubMed] [DOI]
2. Kutuk O, Basaga H. Inflammation meets oxidation: NF-kappaB as a mediator of initial lesion development in atherosclerosis. Trends Mol Med . 2003;9:549-557. [PubMed] [DOI]
3. Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation . 2004;109:III27-III32. [PubMed] [DOI]
4. Magdalena Chmiela et al., Helicobacter pylori vs coronary heart disease - searching for connections, World J Cardiol. Apr 26, 2015; 7(4): 187-203