This is an automatically translated article.
The article is professionally consulted by Master, Doctor Hoang Thi Hoa - Cardiologist - Department of Medical Examination and Internal Medicine - Vinmec Ha Long International General Hospital.Giant cell arteritis is a serious condition, causing many dangerous complications. Let's learn about this disease through the article below.
1. What is giant cell arteritis?
Giant cell arteritis is inflammation of the epithelial lining of the blood vessels. Usually, the disease affects the arteries of the head, especially in the temporal region, and it is for this reason that giant cell arteritis is sometimes referred to as temporal arteritis.
Giant cell vasculitis often causes headaches, scalp pain, jaw pain, and problems with vision. If left untreated, the disease can lead to blindness.
If treated promptly with corticosteroids, symptoms can be alleviated and vision loss is avoided. The condition will gradually improve after a few days of treatment, but even with treatment, the disease often recurs.
Patients will need regular follow-up visits to monitor and treat any unwanted effects from corticosteroid use.
2. Symptoms of Giant Cell Arteritis

Triệu chứng thường gặp của viêm động mạch tế bào khổng lồ
The most common symptom of giant cell vasculitis is a headache, which is often severe and affects both temples. Headaches can get worse, come and go, or go away temporarily.
Usually, signs of the disease include:
Severe, persistent headache, often in the temporal area. Scalp pain. Jaw pain when chewing or opening the mouth wide. Fever. Tired. Unintended weight loss. Loss of vision or double vision, especially in people who present with jaw pain. Sudden permanent loss of vision in one eye. Pain and stiffness in the neck, shoulder, or groin are common symptoms of a related disorder called polymyositis. About half of all patients with giant cell arteritis also have polymyositis.
If new, persistent headaches, or any of the signs and symptoms listed above, see a doctor immediately. If diagnosed with this disease, the earlier treatment intervention is helpful in preventing vision loss.
3. Causes of giant cell arteritis
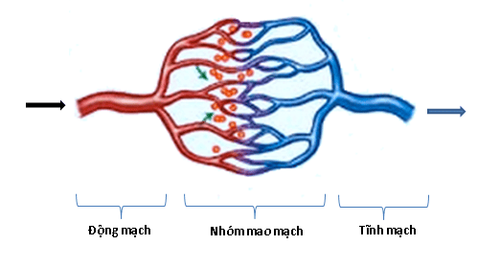
When giant cell vasculitis, the epithelial layer of the artery swells due to inflammation, causing the vessel lumen to narrow, reducing blood flow through the vessel, thereby reducing the amount of oxygen and nutrients needed to supply the blood vessels. supply to tissues.
Nearly any large and medium sized artery can be affected, but giant cell vasculitis most commonly occurs in the arteries of the temporal region.
The exact cause of the disease is unknown, but it is hypothesized that the walls of the arteries are somehow attacked by the body's immune system (autoimmune causes). Certain genes and environmental factors can increase the risk of developing this disease.
4. Risk factors for giant cell arteritis
Viêm động mạch tế bào khổng lồ hầu như chỉ ảnh hưởng đến người lớn tuổi
Several factors can increase the risk of giant cell vasculitis including:
Age: The disease occurs only in adults, and rarely occurs in people under 50 years of age. The majority of cases show signs and symptoms of the disease between the ages of 70 and 80 years. Gender: Women are about twice as likely to get the disease as men. Race and geographical location: The disease is most common in Caucasians of Northern Europe or residents of the Scandinavian peninsula. Rheumatoid arthritis: Having polymyositis increases your risk of developing the disease. Family history: Occasionally occurs in family members.
5. Complications of giant cell arteritis
Giant cell vasculitis can cause serious complications, including:
Blindness: Reduced blood flow to the eye can cause vision loss in one eye, and rarely vision loss in both eyes. . Vision loss is sudden, painless, and often permanent.
Aortic aneurysm: An aneurysm is a bulge (like a bag) at the site of a weak blood vessel, this phenomenon usually occurs in the aorta, a large artery that travels from the mediastinum to the abdomen. An aortic aneurysm can rupture, causing severe and life-threatening bleeding.
Complications of aortic aneurysm can occur several years after a patient is diagnosed with giant cell arteritis, so the doctor will need to monitor the condition of the aorta through X-rays- Routine chest radiographs or other imaging methods (eg, ultrasound, computed tomography,...).
Stroke: Although stroke can occur, it is an uncommon complication of the disease.
6. Diagnosis of giant cell arteritis

Hệ thống máy chụp cộng hưởng MRI tại vinmec
Giant cell vasculitis can be difficult to diagnose initially because early symptoms can overlap with other conditions, and because of this, the physician will need to make a differential diagnosis.
In addition to taking the medical history and presenting symptoms, the doctor will perform a careful clinical examination, especially the temporal artery.
Tests the doctor may order are:
Blood tests: Blood tests can reflect inflammation of the body, including tests such as erythrocyte sedimentation rate, CRP,... Diagnostic imaging Image: Used to diagnose and monitor the patient's response to treatment. Doppler ultrasound: Uses ultrasound waves to visualize the flow of blood in the blood vessels. Magnetic resonance angiography (MRA) and positron emission tomography (PET): Provides detailed images of blood vessels and lesions. Biopsy: For giant cell vasculitis of the temporal artery, the surest way to confirm is to do a biopsy.
7. Treatment of giant cell arteritis
The main treatment for this condition is the use of high doses of corticosteroids (such as prednisone). Because immediate treatment is essential to prevent vision loss, your doctor may prescribe medication before confirming the diagnosis with a biopsy.After a few days of treatment, the patient will gradually feel better. If the patient has lost vision prior to treatment, it will be nearly impossible to restore lost vision. However, if there is no loss of vision, the symptoms will improve.
The patient may need long-term treatment. In addition, giant cell vasculitis is often recurrent, and corticosteroid therapy has many undesirable effects, so patients should have a full examination according to the doctor's appointment for evaluation, monitoring and treatment. intervention (if necessary).
Besides corticosteroids, your doctor may prescribe an immunosuppressant such as methotrexate (Trexall). In addition, the Food and Drug Administration (FDA) of the United States recently approved the use of tocilizumab (Actemra) in the treatment of giant cell vasculitis, but because it is a new drug, The data is not much, so more studies are needed.
References: mayoclinic.org
Master. Hoang Thi Hoa has more than 10 years of experience in the field of Cardiology, especially in the field of cardiovascular emergency and echocardiography. Doctor Hoa used to be the Deputy Head of Cardiology Department of Quang Ninh General Hospital before working at Vinmec Ha Long International Hospital.
If you notice unusual health problems, you should visit and consult with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.