This is an automatically translated article.
The article was made by a doctor of Laboratory - Vinmec Central Park International General HospitalSerology plays a large role in laboratory diagnosis, sometimes with certain inaccuracies in cultures, and when pathogens are urgent or unknown.
1. Take the specimen
In general, serum was the specimen of choice for most trials. Serum was obtained after the clot was removed. Some tests require serum to be heat treated to remove complement. For immunoblotting, plasma can also be used when the primary antibodies remain intact after centrifugation of anticoagulated whole blood with different anticoagulants. The need for each serological diagnosis will be considered.Transport of serum from distant places or by post can use dried sera (69). These specimens may be re-wetted in the receiving laboratory prior to use. Multiple modes of transport have been evaluated and are generally best suited for IgG investigations and especially for screening purposes where large numbers of antibodies are likely. IgM, however, is sometimes sensitive to many if significant manipulations.
Evaluation of mucosal antibodies as markers of infection has been relatively unremarkable. Taking samples is very difficult. For example, detection of antibodies in saliva is common in the serological diagnosis of Helicobacter pylori infection (70,71).

Huyết thanh là bệnh phẩm được chọn lựa nhiều nhất trong hầu hết các thử nghiệm
2. Screening versus deterministic testing
Handling large quantities of serum for any test is a challenge even in the largest laboratories. However, there are standardized and automated commercial type tests that allow diagnostic laboratories to overcome these challenges. Although some tests are not completely specific, like the EIA, they can be designed to ensure that a positive diagnosis is not missed. That is, the diagnostic threshold is adjusted to increase the sensitivity. A test is designed to screen when it is relatively certain that a positive diagnosis is not missed. However, there will be some overdiagnosis, and therefore a positive test from the first screening test must be proven by another test. This test is known as the 'deterministic' test.Immunoblotting is used as a confirmation for the EIA screening test in the diagnosis of viruses, such as hepatitis C and HIV, and the same method is used for the serological diagnosis of Lyme disease. Although the property of immunoblotting that recognizes specific bacterial antigens seems to be appropriate for the definitive test, it is the specificity of the test rather than the formality. In this vein, confirmation using any serological method is possible as long as the test has been shown to have high specificity. For example, for the serological diagnosis of syphilis, non-treponema screening tests are most commonly used and these tests are very sensitive during the active phase of the disease. However, because of the potential for false-positive results, a positive screening test should be followed by tests that identify treponema such as MHTP or FTA (chapter 26). Definitive trials may refer to one or more trials.
In general, testing that is less expensive, easy to perform, and automated is best for screening purposes. Definitive tests are often more cumbersome and expensive. On the other hand, there are many situations where a single serological test can be used for both screening and identification.
3. Evaluation criteria
3.1 Threshold criteria Determining the threshold for a test to be positive or negative must be carefully considered. In general, there are very few serological tests where positive and negative results are absolute. The evaluation of 'grey-zone' is subject to many parameters. The determination of cut-off values is based on comparison of the serological values of the sera of symptomatic and healthy patients, and with the sera of persons who are actually infected as determined by final means of determination. Serological values in between these points are said to be the 'intermediate' region. If the distribution between disease and disease-free is far apart, it is likely that some positive results will be false positives and some negative results will be false negatives. If the distributions of serotypes overlap, the problem of nonspecificity should be of greater concern. These overlapping values can then be treated as 'overlapping' results. If the threshold of positivity is near the high value of the disease group on the distribution curve, the test will increase its specificity but compromise its sensitivity. Conversely, a slope of the threshold near the low value of the disease-free group would lead to improved sensitivity but less specificity (Figure 7). The choice of specificity here must be determined by being aware of missed diagnoses or false positives in any given situation and they are therefore based on experience gained in the application of this field.3.2 Evaluation of utility (Measures of utility) Evaluation of the benefit of serological testing is often described in terms that often provide numbers for comparison. Four key words are commonly used:
Sensitivity: the ratio of true positives to the total number of true positives and false negatives. Indicates the probability of occurrence (detection) in confirmed infections. Specificity: The ratio of true negatives to the sum of true negatives and false positives. Indicates the probability that an uninfected person is not actually infected. Positive predictive value: The ratio of the number of true positives to the total number of true positives and false positives. Indicating the ability to test positive is a true indicator of someone having an infection. Negative predictive value: The ratio of true negatives to the sum of true negatives and false negatives. Indicating the ability to test negative is a true indicator of a person who does not have an infection. Each of the above metrics is usually expressed as a percentage. While those words are often used for the initial assessment and to compare one trial with another, do not forget that the positive predictive value of a test is very dependent on the probability of the disease before (pre- -test) the patient is tested. Therefore, if an infection is common in the population, the positive predictive value of the test will likely be better than that of many positive tests that would actually be obtained from patients with the infection. Conversely, if bacterial infections are extremely rare, even a very sensitive and very specific test may be difficult to apply as a positive test is more likely to occur among people who are not actually ill. Furthermore, the nature of endemic seroprevalence and disease prevalence also influence these values. If infection is common and can be re-infected within a short period of time, the presence of pre-existing antibodies may falsify the results. Even if the disease is rare, but once the disease is present, the antibodies are still present, making it difficult to evaluate the test. Evaluation of serological testing must be emphasized.
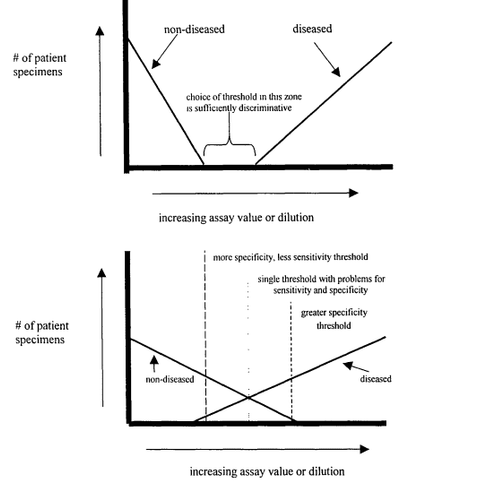
Hình 7: Ảnh hưởng của quyết định ngưỡng xác định tiêu chuẩn ngưỡng (cut-off) trong thử nghiệm chẩn đoán huyết thanh.
4. Quality standards
Most commercial serodiagnostic trials present seropositive and negative controls concurrently with patient sera. In many EIA and CF trials, these sera are needed to ensure that the test is done correctly, and are also needed for self-testing.Using serological tests competently is valuable and will be considered for routine use (72-75).
5. Automation (Automation and robotics)
Many methods can be automated and this can enable fast and cost-effective implementation. The natural development in this area is to be more automated and include more diagnostic tests. However, some serological tests are less commonly used automated and are preferable to manual methods.While performing these diagnostic tests with high automation can be standardized, they also often simplify the input-to-output phase so that specimens are processed quickly and with good results. Fast results, many of which are similar in routine blood cell counts or blood biochemistry tests. There are many aspects to consider such as suitability for use and application value.
6. Point-of-care testing
In medicine, it is desirable to be able to respond as soon as possible and in the shortest possible time. There is, of course, an interest in creating some bedside serodiagnostic tests, or similar fields (76,77). This applies mostly to tests that are easy to diagnose quickly and have some immediate impact in patient care. There have been many attempts towards the application of diagnostic testing for infectious diseases, either serologically or directly for the detection of bacteria. In this regard, much success has been achieved and the promise of becoming technically outstanding.However, the Several point-of-care tests, are commercially available and convenient to use, but experience with them is less sensitive (some significantly lower) than the pre-existing standard. Promising definitive trials for clinical application are needed. There are indeed few studies that clearly show the economic benefits of using serological diagnostic tests in general. Furthermore, point-of-care tests are often designed with the hope of reaching less skilled testing teams. To make simple tests usable by less skilled people, a new version is released. For example, simply without experience the assessment of latex agglutination can be highly misleading leading to misdiagnosis. It is sometimes necessary to carefully compare bedside rapid tests with standard methods to ensure that the test is correct to which it is applicable.
Invite you to follow the document on Serological Diagnosis of Infections by Doctor Tran Thi Ngoc Anh including:
Serological Diagnosis of Infections Antigens and antigenic variation Antigen relationship Voidness specificity of the humoral immune response Summary of serodiagnostic methods - Part 1 Summary of serodiagnostic methods - Part 2 General aspects of utilization in hematology Bar The Complicated Situation in Serological Diagnosis Source: Nevio Cimolai
Children's and Women's Health Center of British Columbia, Vancouver, British Columbia, Canada