This is an automatically translated article.
The article was made by a doctor of Laboratory - Vinmec Central Park International General Hospital
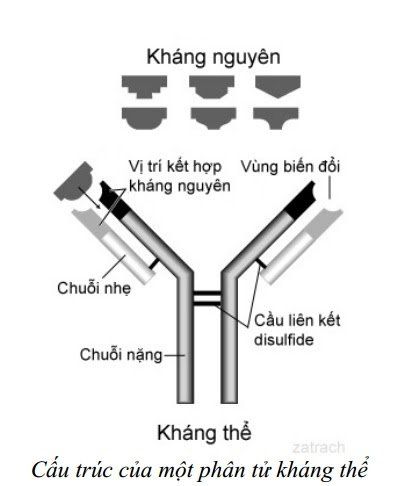
Serological diagnosis has a functional basis of the humoral immune response to infection. With regard to past and present considerations, there is precedence over the measurement of the cell-mediated immune response to infection.
1. Why use serology?
Serological diagnosis has been favored for its considerable benefit and continues to be an important choice of application despite recommendations that use molecular biology and diagnostic dependencies. From the past, serology plays a large role in laboratory diagnosis, sometimes with certain inaccuracies in culture methods, and when urgent or unknown pathogens are present. . Indeed, for some difficult pathogens, serologic diagnosis is often the first-line approach. For pathogens that cannot be cultured, the ability to multiply the bacterial genome specifically and where antigens are expressed, especially proteins, in vitro serology is suggested as proof evidence.
Chẩn đoán huyết thanh là lựa chọn đầu tiên trong chẩn đoán bệnh nhiễm khuẩn
There are many reasons why serology is the first or mandatory option in the diagnosis of bacterial infections:
Bacteria cannot be cultured, such as syphilis. Bacteria can be cultured but the results are slow or the technique is difficult, eg bartonellosis. It is difficult to obtain enough bacteria to culture (live bacteria) or perform genetic tests, for example Lyme disease. In an infected place, it is difficult to get samples to perform other methods. The pathogen is new but difficult and serodiagnosis is the easiest method for the new agent. The serological response is unique to the pathogen and the serologic epidemiology is extremely low. The serological response is very constant and when found, the diagnosis of infection is high. Serological testing can often be reactive when the patient is ill. Serological diagnosis may be the sole criterion for evaluating other, even reference, methods. The type of application of serology can be easy to implement and easy to automate for easy implementation with large sample numbers. Serological testing can be easier and more cost-effective than other methods, especially if the facility is equipped with only moderate equipment. Serological methods are needed as an adjunct to culture, gene detection, or other methods that increase the diagnostic sensitivity of the patient cohort in general. Serology is good for screening Serology may not be needed for diagnosis, but is used to determine immunological status since its presence is necessary to rule out a disease. The decision to choose a serological method is often a consideration for many reasons, not just one. Table 1 lists some examples of infections and the value of serological diagnosis.
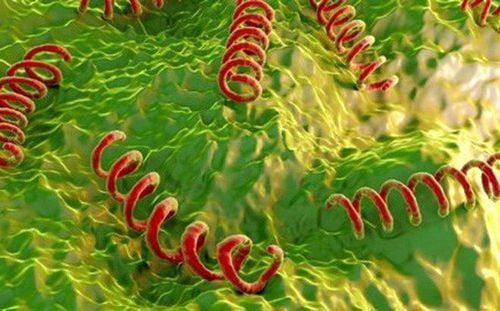
Vi khuẩn giang mai không thể cấy được nên cần sử dụng phương pháp huyết thanh
2. Reasons for not using serology
Similar to the reasons for using serological methods, there are many reasons for using other diagnostic methods. These reasons include:
Infection progresses rapidly (in hours to days) and insufficient time to induce an immune response (requires at least 5-10 days). The serological response may be slow in some patients and persists into the 2nd and 3rd week of illness. There may be a high frequency of serologic epidemiology in the population, thus leading to nonspecificity (many preexisting antibodies may be due to resident bacteria). Inoculation or gene detection or other diagnostic methods may allow more time or more definitive results. Infections can be repeated (reinfection or relapse) and an immune response is more pre-existing than present in the IgM response, thus making IgM detection difficult. Undue delay in performing a serological test may occur if sample transfer is required.

Phương pháp cấy cho kết quả xác đáng hơn.
Re-sampling is required to compare remission sera with acute phase sera to determine immune response to infection. Age-related immune response. Nonspecificity, cross-reactivity with other bacterial or non-bacterial agents. The immune response may be variable and activated to different antigens for different patients (eg, variable response to ASOT or anti-DNAase in streptococci infection) Routinely measured serum antibody response may not reflect the response to mucosal or other site infections. Infections may be the only casualty where high levels of antibodies, such as IgM, may be seen as the result of infection from previous months rather than recent. Empiric antibiotic therapy is often used despite serological testing. The disease is known to be mild and diagnostic testing is not significant, testing is rarely performed. Serology plays a very minor role compared to other methods. Price can be a concern for less developed places. Using serological testing may simply be temporary pending the development of new and more effective methods. There is a clear contraindication because of the specificity of the test (eg, anti-complement in the fixation test, anti-erythrocyte antibody in the indirect agglutination test, non-specific agglutination in the individual agglutination test). part) There is too much variation in the different test runs. Response may be nonspecific when heterophil antibodies are evaluated. The test may not travel from place to place (cannot be portable) Assessing response in infants can be difficult because of the mother-to-child transmission of antibodies. Using serodiagnosis can make the arguments listed in the table below:
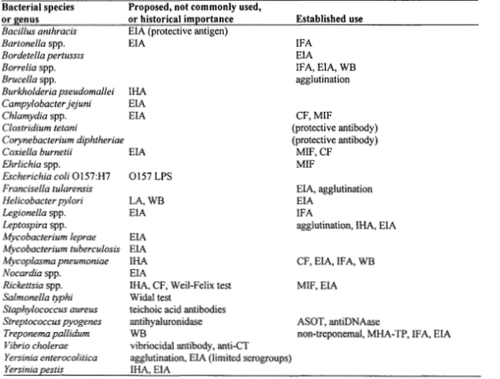
Bảng 1: Vai trò của chẩn đoán huyết thanh trong bệnh nhiễm khuẩn. Những chữ viết tắt: EIA-enzyme immunoassay; IFA-indirect immuno fluorsecence; WB-Western Blot; IHA-inderect hemagglutination; CF-complement fixation; MIF-microimmunofluorescence; ASOT-antistreptolysin O; CT-cholera toxin; MHA-TP: micro-hemagglutination assay cho T. pallidum
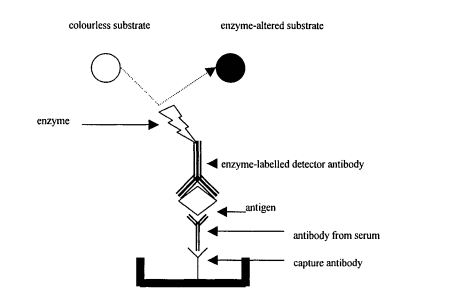
3. Common serological diagnostic methods
There is much concern about the need for serological methods whether used for bacterial infections or infections with other agents. These points are variously acknowledged as routine methods in serological diagnosis of infectious diseases.
If the humoral response is measured within 7-10 days of infection, many patients will be disease-free in the presence of a serological response. A single specimen with sufficient titers does not appear in less than 5-7 days. Therefore dual sera is desirable for titre comparisons; The first sample alone has no diagnostic value, but the second serum sample (in remission) to compare titre changes. The change in antibody titres between the 2 samples usually requires 5-7 days, although 2 weeks will ensure this if the first serum sample has a low titer. If the patient is late, the 2 titres may be roughly equivalent but at a high level. On the other hand, patients arriving late after several weeks of illness may show signs of a decrease in titres. It is of interest that the change in titre between the early and late samples is at least as large or as significant as it is, usually four times. The 2x titre change is not significant due to inherent error in such breakpoints; However, it must be understood that there is a small percentage (usually < 5% and often depending on the method used) that the titre can change 4 times due to error. Except, the ASOT change in Streptococcus pyogenes infection was significant even though it was less than 4-fold (1).
Use of only one serological titre will depend on the normal distribution of serological results in the unaffected population. The specificity of the significant titre will be weighed against the sensitivity of detection against the nonspecificity associated with the normal distribution.
IgM được xác định tốt nhất khi nhiễm khuẩn ở giai đoạn sớm
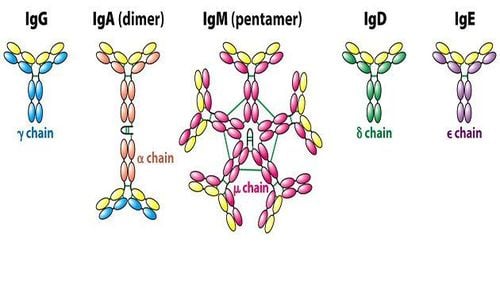
Early sepsis is best defined by IgM response. Normally, IgM is detectable for 7-10 days depending on the nature of the infectious agent. For example, IgM responses are frequently observed in respiratory Mycoplasma pneumoniae infections among otherwise normal individuals (2). In contrast, it is not uncommon to see a slow IgM response in early Treponema pallidum infection (3). Although EIA, IFA, radioimmunoassay, and immunoblotting can be specific for detecting IgM responses, many other tests measure fortuitous combinations of IgG and IgM, such as complement fixation and agglutination assays. CF). The IHA test is primarily for the measurement of IgM (4) and the neutralization test for the measurement of IgG beyond the middle stage of infection (5).
The humoral response is characterized using patient serum rather than other specimens. Serum administration requires adequate immunity to be achieved whether the agent penetrates deep tissues or is due to the mobilization of an immune response (such as antibodies produced by B cells) from another site of infection to the cell reservoir. immunity. However, for some infections, there is a more mucosal rather than systemic response.
It is desirable to have a unique immune response with little opportunity for either prior recognition of the antigen or previous infection). When many agents are derived from resident bacteria and when infection with other agents is recent, the immune response is more likely to be anamnestic than primary. The IgM response may be poor or absent in many reinfection responses, and in which case IgG predominates.
Please follow Dr. Tran Thi Ngoc Anh's set of documents on Serological Diagnosis of Infectious Diseases including:
Serological Diagnosis of Infections Antigen and Antigen Variation Antigen Relationship Nonspecificity The effect of the humoral immune response Summary of serodiagnostic methods - Part 1 An overview of serodiagnostic methods - Part 2 General aspects of utilization in serology The Complicated Situation in Serological Diagnosis Source: Nevio Cimolai
Children's and Women's Health Center of British Columbia, Vancouver, British Columbia, Canada