This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
A high degree of clinical suspicion is required for a definitive diagnosis of gastrointestinal amyloidosis. Because of the rare condition with nonspecific signs and symptoms at the time of presentation, these patients often undergo extensive and unnecessary testing to determine the etiology of the clinical presentation.
Gastrointestinal amyloidosis should be included in the list of possible differential diagnoses in patients with nonspecific gastrointestinal symptoms and a medical history of disorders commonly associated with amyloidosis. , such as plasma cell disorders, chronic renal failure on dialysis, and other chronic inflammatory conditions (eg, rheumatoid arthritis and inflammatory bowel disease). A positive family history of amyloidosis should also alert the provider to suspected gastrointestinal amyloidosis.
1. Laboratory tests
Tests in these patients may show anemia, mildly elevated ALP levels, acute phase reactant elevations (due to underlying chronic inflammation), and malabsorption deficiencies. Diagnosis by radiology and CT scan in gastrointestinal amyloidosis is usually nonspecific. Some features commonly seen on computed tomography (CT) or magnetic resonance imaging (MRI) include: (1) Diffuse or nodular wall thickening of the involved bowel; (2) The dilution depends on the degree of mobility impairment; (3) Presence of fluid levels in dilated loops of bowel; (4) Intestinal stenosis secondary to amyloid infiltration or ischemia; (5) Decreased tissue density due to calcifications or mucosal ulcers; (6) Presence of cancerous growths or masses; (7) Mesenteric thickening or lymphadenopathy; and (8) Decreased hepatic attenuation with or without areas of calcification (Ultrasound may show liver echogenicity with foreign body).
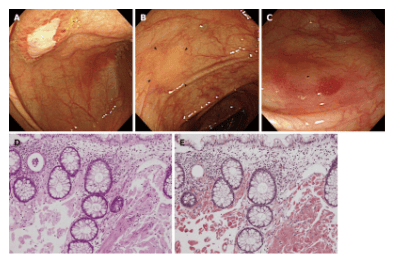
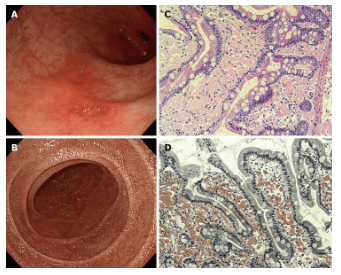
Although radiological investigation may provide clues to extent and region involved, the gold standard test to establish the diagnosis of gastrointestinal amyloidosis is tissue biopsy followed by Congo red staining and visualization. under a polarized light microscope. Based on the patient's symptoms, an upper gastrointestinal endoscopy or colonoscopy should be performed to obtain a biopsy sample. As mentioned earlier, the site for the highest diagnostic results from biopsies in the gastrointestinal tract was found to be the duodenum, followed by the stomach, rectum, and esophagus.
Liver biopsy may also be performed to confirm hepatic invasion of amyloid proteins; however, transcellular route should be used to prevent fatal bleeding complications. In addition, the study by Yen et al. reported biopsy-negative disease in 55% of patients. However, these patients met the Rome IV criteria for some bowel dysfunction, but only 23.2% underwent additional diagnostic studies to evaluate the function of the gastrointestinal tract. (such as oesophageal or anorectal measurement, capsule endoscopy, or gastric emptying study). Therefore, the authors recommend that additional diagnostic studies are needed to evaluate movement disorders in patients with clinical features of gastrointestinal amyloidosis but negative biopsy results.
Histopathologic picture
Amyloid filaments appear as amorphous, eosinophilic deposits on conventional hematoxylin-eosin-stained preparations, which can sometimes be confused with hyaline or sclerotic changes . Therefore, Congo red staining with the characteristic apple-green birefringence of Congo red staining residues under polarized light has been considered the gold standard for definitive diagnosis since its inception. However, although the Congo red staining method has high sensitivity and specificity, false negative results may be seen due to the amount of amyloid deposition in the tissue, the age of the residue, the thickness of the sections for visualization. , fixation of tissues on the slide, or the staining procedure itself. Therefore, newer methods are being developed to act as an adjunct to the diagnosis. Digital-enhanced hematoxylin-eosin polarization (DRHEP), a newly introduced technique that uses both conventional light microscopy and digital imaging, can detect weakly non-refractive birefringence. detected through the microscope. Although the use of DRHEP is currently limited to kidney biopsies, its role in gastrointestinal amyloidosis is currently under investigation.
2. Treatment
Once the diagnosis of gastrointestinal amyloidosis is established, the biopsy specimen should be further analyzed to identify the subtype of amyloid deposition, which can then help guide treatment. The management of GI amyloidosis includes: Symptom management Symptom control in patients with gastrointestinal amyloidosis is tailored to the clinical presentation. In patients with symptoms of dysfunction (stagnation syndrome), dietary modification, adequate hydration, and use of adjunctive and antiemetic drugs should be considered. Dietary changes include frequent, liquid, small-volume, or homogenous foods with low fat and soluble fiber content along with nutritional supplements as needed. Motor stimulants such as metoclopramide, erythromycin, or domperidone (if indicated) are primary therapy for dyskinesia. Parenteral nutrition is indicated in cases of severe chronic gastrointestinal disorders. Patients with dysphagia can be successfully treated with balloon dilation. For patients with diarrhea or abdominal distension, antidiarrheal drugs such as loperamide should be used.
Empiric antibiotic therapy should be considered in patients with diarrhea and suspected bacterial overgrowth. In patients with severe diarrhea associated with protein-losing enteropathy, the literature reports a good response to corticosteroid and octreotide therapy. Management of GI bleeding includes appropriate staging, supportive measures, volume resuscitation if necessary, and source control through vascular ligation of the bleeding. Surgical intervention may be necessary in cases of severe obstruction, uncontrolled gastrointestinal bleeding, or intestinal ischemia. Patients with macroglossia causing airway obstruction or obstructive sleep apnea may need to have part of the tongue removed to relieve symptoms.
Treatment of the underlying condition of systemic amyloidosis
There is no specific treatment regimen for the management of gastrointestinal amyloidosis . Treatment varies considerably depending on the cause and type of amyloid protein deposition in the tissues. Current management strategies based on the type of amyloid deposit available in the literature include:
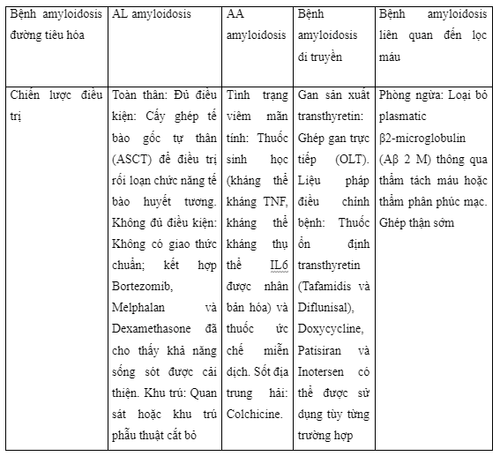
Light chain amyloidosis: This therapy targets the production of monoclonal immunoglobulin light chain through its job of eliminating plasma cells. Autologous stem transplantation is the criterion for plasma cell dysfunction in eligible patients. For patients ineligible for autologous stem cell transplantation, location is unclear; however, the use of Bortezomib, Melphalan, and Dexamethasone combined data has shown complete hematological response and survival rates. Daratumumab plug-in (the single line of the CD38 against user) to therapy bortezomib-based therapies have been evaluated, but the results remain unpublished. Furthermore, the induction of resistance to the fully cloned monoclonal IgG1 amyloid component P (Dezamizumab) was also evaluated for AL amyloidosis.
Serum Amyloidosis:
Therapies are specifically directed at checking the underlying disease, thereby helping to reduce acute phase reactivity and serum amyloid A protein production. Colchicine is used in patients with Mediterranean Fever. Biologics (active against inflammatory cytokines such as TNF-alpha, IL-1, and IL-6), cytotoxic agents, and immunosuppressants have an important role in the management of such situations. Inflammatory state of a hidden nature in the form of inflammation, inflammatory bowel disease and inflammation in other diseases.
Inherited amyloidosis:
Therapy aimed at removing a gene that alters the source of the protein. The liver produces most of the circulating TTR in the body. Direct liver transplantation can be used to reduce variable protein production in patients where the liver is the culprit. Various disease-modifying approaches such as TTR Stabilizers (Tafamidis and Diflunisal), Doxycycline, Patisiran and Inotersen may also be considered on a case-by-case basis.
Dialysis-associated amyloidosis:
There is currently no medical or pharmacological therapy for dialysis-associated amyloidosis [60]. Prevention and treatment include plasmatic removal of Aβ 2 M through hemodialysis or peritoneal dialysis using ultrapure dialysis or with more biocompatible and high-throughput membranes [60] . Furthermore, early and successful kidney transplantation leads to a decrease in Aβ 2 M levels, which after a few years can lead to degradation of deposited amyloid proteins.
Treatment of localized amyloidosis:
It is characterized by the deposition of amyloid AL confined to the gastrointestinal tract. For asymptomatic patients, intervention may not be needed and observation may be key; however, patients with recurrent or severe symptoms may require focal surgical resection.
3. Prognosis
The prognosis of gastrointestinal amyloidosis depends on the extent of the gastrointestinal tract injury, the amount of deposition, and the type of amyloid deposition. The literature reports that patients with light chain amyloidosis and gastrointestinal disease have worse quality than those without GI involvement. In addition, patients with gastrointestinal amyloidosis had different organ involvement, increased number of bad factors, and more severe disease progression compared with patients without gastrointestinal involvement. Patients with serum amyloidosis are reported to have a better mean exit outcome. Liver entry is associated with poor prognosis and increased mortality, particularly in patients with baseline jaundice and those with high serum direct bilirubin levels (> 2 mg/dL)
Conclusion
Amyloidosis is characterized by extracellular deposition of autologous fibrous proteins that assemble into three-dimensional ß pleated sheets arranged in an anti-parallel fashion. Patients with gastrointestinal amyloidosis often present with fatigue, dizziness, anorexia, weight loss, gastrointestinal bleeding, malabsorption, protein-losing enteropathy, or gastrointestinal disturbances. chronic chemistry. Amyloid protein infiltration in the liver can also be seen, often with hepatomegaly and mildly elevated ALP. Hepatic jaundice (elevated direct bilirubin >2 mg/dL) is associated with a poor prognosis. Radiographic investigation is usually nonspecific, and a definitive diagnosis is established by tissue biopsy followed by Congo red staining.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.