This is an automatically translated article.
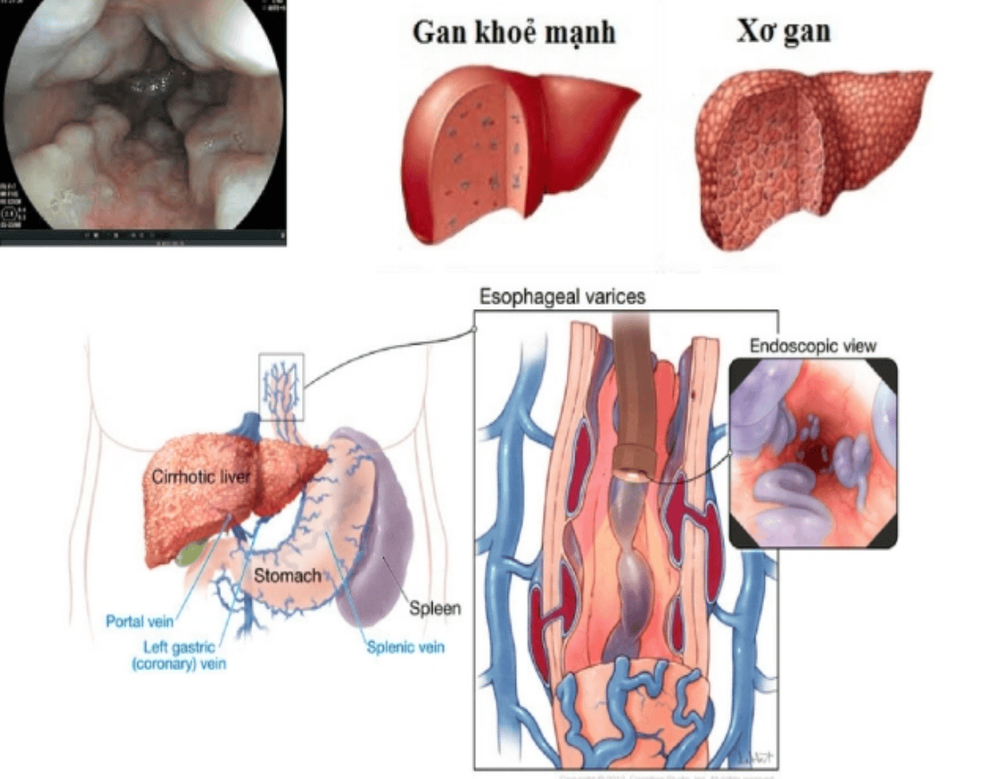
The article was written by Doctor Mai Vien Phuong - Gastrointestinal Endoscopy, Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalThe main cause of portal hypertension is cirrhosis - the end stage of any chronic liver disease. Patients with cirrhosis present clinically with 2 main syndromes: hepatic dysfunction syndrome and portal hypertension.
1. Mechanism of formation of gastric esophageal varices
1.1 Portal hypertension Portal hypertension or for short, portal hypertension is a medical condition that increases pressure in the venous system that carries blood from the viscera to the liver. However, portal hypertension is not merely an increase in pressure in the venous system but rather an increase in the pressure gradient between portal inflow and outflow of the hepatic vein.
The primary cause of portal hypertension is increased resistance to vascular flow due to structural changes in the liver parenchyma due to fibrous tissue formation and the formation of neoplastic liver nodules through the inflammatory process.
In addition, recent findings suggest that portal hypertension is aggravated by vasoconstriction of the intrahepatic vascular system due to a decrease in local NO production with increased NO production in the liver. visceral and peripheral vasculature, causing vasodilation resulting in increased blood flow and volume. The formation of collateral loops with the aim of reducing portal pressure has been unsuccessful for two reasons:
There is an increase in portal venous outflow due to splanchnic vasodilatation concomitant with the formation of the portal vein. complete system. The resistance of the collateral circulation in patients with cirrhosis is greater than the resistance of the blood vessels in the liver in the normal person. Therefore, an increase in portal pressure in patients with cirrhosis is the result of two main phenomena: increased resistance to flow through the portal system (intrahepatic and collateral circulation) and increased flow. in the door system.
2. How to assess portal pressure
Direct portal pressure assessment is difficult to perform due to its invasive nature, complexity, and complications. Instead, portal pressure is measured indirectly through the hepatic venous pressure gradient (HVPG).
This method is less invasive, easy to implement, and still accurately reflects the value of portal venous pressure. The value of HVPG is calculated as the hepatic venous pressure (WHVP) minus the free hepatic venous pressure (FHVP).
Normal value of HVPG from 1 to 5 mmHg, above 5 mmHg is called portal hypertension. Portal hypertension is clinically significant when the hepatic venous pressure gradient is greater than 10 mmHg.
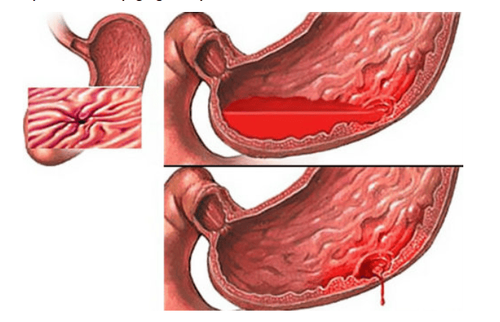
3. Mechanism of esophageal varices rupture
The most accepted mechanism of varicose vein rupture is the explosive mechanism in which the decisive cause is an increase in hydrostatic pressure inside the varicose with hemodynamic changes and associated consequences : Increase in size and decrease in thickness of varicose veins.
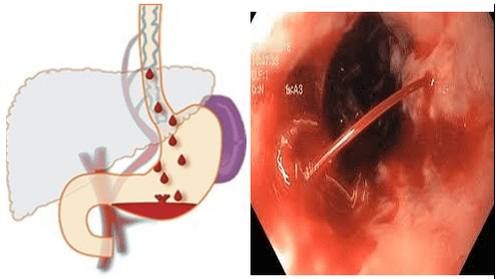
3.1 Role of hemodynamic factors Increased portal pressure Many studies have shown that varicose veins rupture only when the HVPG gradient is greater than 12 mmHg. In contrast, when HVPG is less than 12 mmHg by drug therapy or TIPS, the risk of varicose veins rupture is almost non-existent. Even varicose veins can decrease in size and disappear. Similarly, when the HVPG decreases by more than 20% of the initial pressure, the risk of varicose veins rupture is very low. Increased pressure in the varicose veins Rigau J.'s study showed that the pressure in the dilated veins was significantly related to portal pressure. At the same time, patients with bleeding from varicose veins had higher pressures in the varicose veins than patients without bleeding even though portal pressures were the same. Feu F.'s study showed that propranolol, in addition to lowering portal pressure, also significantly reduces pressure in varicose veins. Changes in intra-abdominal pressure (patients with ascites or ascites) have an effect on varicose veins, increasing or decreasing the risk of bleeding. As intra-abdominal pressure increases, portal pressure as well as pressure in varicose veins increases, increasing the risk of bleeding. In contrast, when puncture ascites reduces intra-abdominal pressure, reduces portal and varicose veins, and reduces the risk of bleeding. The pressure in large varicose veins is higher than in small varicose veins. This suggests that it is possible that the pressure in the varicose veins contributes to the size of the varicose veins. Pressure in varicose veins is related to the risk and severity of bleeding. 3.2 Size of varicose veins Patients with bleeding due to rupture of esophageal varices have larger varices size compared to patients without bleeding. Furthermore, the risk of bleeding from varicose veins is directly related to the size of the varicose veins.
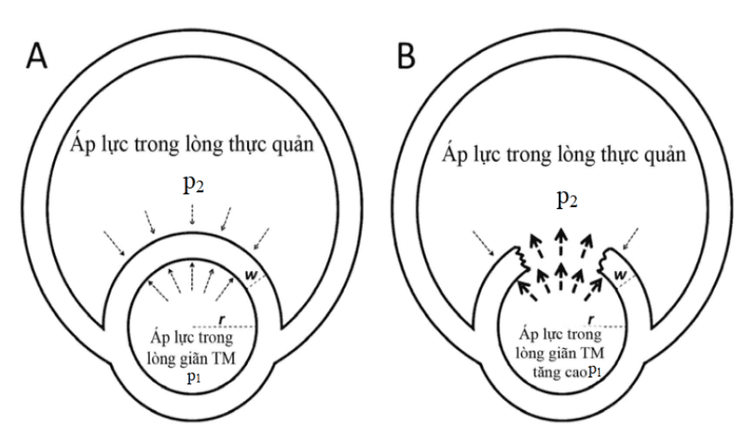
3.3 Pressure on the wall of a varicose vein A varicose vein ruptures when the pressure inside the vessel is greater than the resistance of the vessel wall. When the pressure increases, the elasticity of the vessel wall also changes to protect the vessel wall. But when the pressure is too high, the elasticity of the vessel can not be increased any more, the phenomenon of vascular rupture will occur.
4. Anatomical location of varicose veins
The most common site of varicose vein rupture is the lower third of the esophagus, the anatomical location of the barrier zone (the area from the gastroesophageal junction to the upper 2 - 3 cm) and the easy area. rupture (perforating zone, 3 - 5 cm junction of the barrier zone) of the esophageal vein where the veins are located superficially at the choroidal site. In these areas, esophageal varices do not have a supportive outer tissue layer, so they are gradually prone to dilation and rupture under the impact of portal hypertension.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Nguyen Xuan Hien (2009), “Research on endoscopic images of esophageal mucosa in cirrhosis patients”, Vietnam Journal of Gastroenterology, p. 1075-1079. 2. Tran Van Huy, Pham Van Linh, Pham Minh Duc (2006), "Efficacy of endoscopic rubber band ligation in the treatment of bleeding due to ruptured esophageal varices", Practical medicine, 532 , p. 23-29. 3. Tran Van Huy (2006), “Efficacy of endoscopic rubber band ligation combined with propranolol in preventing recurrence of esophageal varices rupture in patients with cirrhosis”, Vietnamese Medicine, Hepatology. secret, p. 140-149 Study on the effectiveness of esophageal varices ligation in combination with propranolol in the prevention of recurrent bleeding and its impact on portal hypertension due to cirrhosis (2014). Tran Pham Chi, Doctor of Medicine Thesis, Hue University of Medicine and Pharmacy Nguyen Ngoc Thanh, Nguyen Thuy Oanh (2012), "Evaluate the effectiveness of methods to prevent recurrent esophageal varices rupture by elastic ligation combined with propranolol. ”, Journal of Medicine Ho Chi Minh City, 16 (3), p. 29-35.