This is an automatically translated article.
The article was written by a doctor of Laboratory - Vinmec Central Park International General Hospital.White discharge is the mucus secreted from the lining of the vagina and cervix of women. Physiological white blood is clear white, slightly slimy, tough, but easy to break, slightly sticky like egg white, has no odor or slightly fishy, does not smell and does not cause itching. The following article will provide information about the smear test - white blood staining in detecting the causative agent of vaginitis.
1. Overview of white blood cells
Physiological white blood: is the mucus secreted from the vaginal mucosa and cervix of women. When entering puberty, the female ovaries gradually develop and secrete fluid, this fluid causes the genitals to start producing hormones, thereby leading to the appearance of white blood cells. . Physiological white blood is clear white, slightly slimy, tough, but easy to break, slightly sticky like egg white, has no odor or is slightly fishy, does not smell and does not cause itching, small quantity - increases with concentration Estrogen increases.Pathological leucorrhoea: when there is vaginitis due to many agents, depending on the infected agent, white blood also has different properties and colors:
Inflammation caused by Gardnerella vaginalis: Yellow thin white, grayish white very foul fishy smell of rotten fish, evenly coated in the vagina. Inflammation caused by Candida albicans: Yellow, opaque, thick, lumpy like curd, yogurt, lime mortar. Bad smell, large quantity, with vulvar itching. Inflammation caused by Trichomonas vaginalis: Yellow, green, foamy, fishy, large quantity accompanied by vulvar itching.

Huyết trắng sinh lý là chất dịch nhầy được tiết ra từ niêm mạc âm đạo và cổ tử cung của nữ giới
2. What kind of vaginitis can be detected by the smear test - white blood staining?
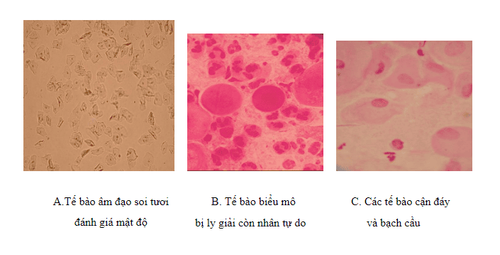
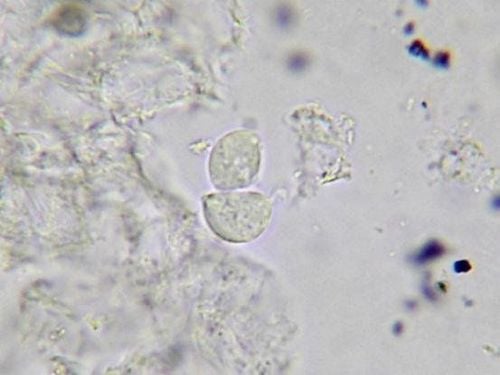
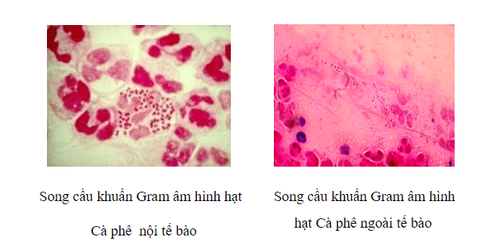
2.1 Visceral examination Can detect fungi, flagellate Trichomonas Clue cells “Clue cell” Bacterial vaginitis AV (Aerobic vaginitis – Aerobic) Vaginal epithelial cells (Squamous cells) 2.2 Gram stain Survey Gram-stained specimens allow to identify the shape, arrangement, and gram-negative and gram-positive staining properties of bacteria, to orient the diagnosis of pathogens such as gonorrhea, bacteria that cause acanthemia. Soft and identify bacterial vaginosis... Gonorrhea: Under KHV, bacteria are coffee bean-shaped, standing in pairs, gram-negative, located inside white blood cells, sometimes outside white blood cells. . When looking at the above properties of bacteria, only note: "Found a gram-negative cocci, coffee bean-shaped inside the cell (or outside the cell) in gonocoque form" and also noted the presence of cells. pus cells and other bacteria. G. vaginallis was formerly known as Haemophi. vaginalis or Corynebacterium vaginalis: spherical bacilli, changing Gram's color. Clue cells "Clue cells": are vaginal epithelial cells covered with a lot of bacteria (mainly Gadnerelia vaginalis) densely concentrated, to the extent that the cell border is not clear, accounting for more than 20% of the cells. epithelium. Valuable in the diagnosis of bacterial vaginosis. Bacterial vaginosis (BV) Bacterial vaginitis (Aerobicitis) Normal microflora Lactobacilli Bacterial causes that share a common microbiological feature are changes in the microbiota. normal (microbiome or microflora or microflora) vaginal tract.3. How to read the white blood smear result table
Macroscopic observation and optical microscopy direct survey of genital tract specimens.3.1. Vitroscopy without background: is a method of microscopy to close the causation, with the specimen placed in a drop of physiological saline on a slide, pressed under a lamelle and observed under a 40X objective. find Trichomonas , fungi and Clucel cells:
Positive result (+++) or more means disease. Vaginitis caused by a yeast infection usually has many polymorphonuclear white blood cells.
Trichomonas vaginalis This is a single-celled parasite, moves by cilia, lives in the vagina. On fresh microscopic specimens, Trichomonas vaginalis are large flagella, especially mobile, both round and backward, pear-shaped in shape. or pea, has a ty axis. The cytoplasm has many vacuoles. There is one corpus callosum, the corpus callosum has 3-5 lower cilia, the large nucleus is located near the head, common in female patients.
When seeing flagella, if on average each 40X objective field, you can see:
1 - 2 flagella are positive (+) 3 - 5 flagella are positive (+ +) > 5 flagella are positive (+) ++). If flagellate is found, there is an infection, often accompanied by leukocytosis.
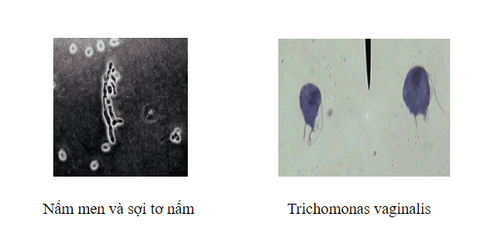
Hình ảnh Nấm men, sợi tơ và Trichomonas vaginalis
< 25 cells/VT (+): Normal 25-100 cells/VT (++): Td and identify with other agents. >100 cells/VT (+++): Abnormal Cell density: More or less depends on time of menstrual cycle and inflammation.
AV vaginitis (Aerobic vaginitis - Aerobic) using the method of fresh microscopy in physiological saline and vaginal fluid specimens was evaluated at objective 40: LBG (Lactobacillary grades) = I is no there are other bacteria mainly lactobacilli morphology changed; IIa mixed bacteria but lactobacilli still dominate; IIb mixed bacteria but the percentage of lactobacilli is severely reduced due to increased number of other bacteria; III little or no lactobacilli due to overgrowth of other bacteria. WBC count:
Score 0 is equivalent to < 10 BC / 40 ; Score 1 is given for cases with > 10 leukocytes/40 and leukocyte/epithelial ratio < 10; A score of 2 is given in cases where there are > 10 leukocytes/40 and leukocyte/epithelial ratio 10. Toxic leukocyte (toxin) ratio is based on the granular characteristics of white blood cells due to excessive hydrolytic activity. (granular appearance due to abundant lysozymic activity). Score 0 without these cells; 1 if toxic leukocytes ≤50% white blood cells; and 2 if >50% of the leukocytes are toxic.
Bacterial background is given 0 if the microfield background is unremarkable or shows fragments and inert nuclei of lysed epithelial cells; score 1 if lactobacilli are very short or with short bacilli (unlike lactobacilli); and 2 if predominately cocci or cocci are seen.
Calculate AV score:
It is the simplest method to distinguish between two types of vaginal microbiota abnormalities: anaerobic (BV) and aerobic (AV) vaginitis. Using the composite score for quantitative results is easy to evaluate, it is also easy to assess the risk and predict the effects on the fetus and mother such as preterm birth, premature rupture of membranes, Premature rupture of membranes, postpartum infection ... Because the effects of aerobic bacteria are considered very dangerous for pregnancy and childbirth, but there is no effective tool to measure.
3.2. Gram staining results Interpret the results under the X100 objective microscope.
Gonorrhea Gram staining results for gonococci are highly valuable in cases of acute urethritis
in men. Cases of urethritis complicated by gonococcal counts are very rare and cannot be definitively determined by Gram staining alone. It is necessary to do other indications such as culture or PCR (Polymerase chain reaction). In women, the Gram stain for gonorrhoea is only valid in the following cases: the smear test is positive and the patient has clinical symptoms of cervical gonorrhea infection. . The test is only useful for screening when the patient is asymptomatic, and direct testing is of little value when detecting gonorrhea in the pharynx and anus.
Heamophilus ducreyi is a rod-shaped bacillus, poorly stained, and confirmed as one of the causes. Genital ulcers in chancroid.
Shave genital sores to make smears. Gram stain or Toluidine Blue, or methylene blue Gram stain: Heamophilus ducreyi is pale pink, short rod-shaped with parallel edges, rounded at both ends and clearly colored for a distinctive image compared to other bacteria. Arranged in a row, or in the shape of a school of fish.
Toluidine Blue staining: Heamophilus ducreyi is blue, the middle part is bright and dyed at both ends very typical,
The real etiology of BV is not really clear yet, but BV is related to changes in the microbiome (ecology) vaginal ecology) causes the overgrowth of certain bacteria, including Gardnerella vaginalis and other anaerobes. Overgrowth of these BV bacteria replaces the normal microflora of the vaginal bacteria, Lactobacillus .
Nugent criteria: vaginal fluid is taken with a cotton swab from the vaginal wall and then spread on the slide for staining, assessing the shape of bacteria cells on the oil objective (100) as follows:
(Number of /field 100)
Calculate points according to Nugent and return the result.
AV-associated vaginitis (Aerobic vaginitis - Aerobic) KS directly on Gram-stained specimens of vaginal fluid to diagnose bacterial vaginosis:
Due to disrupting the dominance of Lactobacillus but often accompanied by obvious inflammation more pronounced than BV and the presence mainly of common bacterial pathogens such as B streptococcus, (S. agalactiae), Enterococcus faecalis, Escherichia coli, and S. aureus.
From a clinical perspective, the results of direct investigation of Gram-stained smears on vaginal and cervical swabs provide clinicians with necessary and effective information for diagnosis, evaluation, and follow-up. Follow-up treatment of bacterial vaginosis.
Difference between AV and BV:
Evaluation on staining slides: 100X oil objective, evaluate and determine the presence of cells and bacteria, report white blood cell count and Gram characteristic of VK.
Normal vaginal discharge specimen:
Mainly Gram-positive bacilli (Lactobacillus ) Normal epithelial cells Few white blood cells (< 5 white blood cells/field). Vaginitis not due to gonorrhea:
If <=5-10 white blood cells / field Gram-positive bacilli (Lactobacillus) No intracellular Gram-negative diplococci. Vaginitis caused by Gardnerella vaginalis :
If <5 white blood cells / field No Gram-positive bacilli ( Lactobacillus ) Many small Gram-negative bacilli around the cell with other bacteria such as Gram-negative cocci, Gram-negative bacilli [ -], Gram negative curved. Suspected Chlamydia trachomatis: > 10 WBCs/field:
Cervical smear: More than 10 WBCs/field and presence of intracellular or extracellular Gram-negative dicycytopenia can confirm over 98% of patients with gonorrhea:
If polymorphonuclear leukocytes and granular Gram-negative cells are seen Intracellular coffee suggests acute gonorrhea. If there are no or few white blood cells and few extracellular coffee bean-shaped Gram-negative leukocytes, chronic gonorrhea may be present. If you see Gram-negative bacilli, think Coliform.
If the density of Gram-positive cocci or Gram-negative bacilli is too much with an increase in white blood cells, it is thought to be the causative agent of vaginitis.
However, Gram stain results cannot be sure that the patient has gonorrhea.
Summary: Bacteria are assessed according to 3 conditions:
1. Status I:
Bacterial vaginosis Negative (BVN) Presence of a single population of Bactobacilli, which are large, long rod-shaped Gram-positive bacilli.
2. Condition II:
Bacterial vaginosis Indeterminate (BVI) presence of many types of bacteria characterized by a decrease in Lactobacilli populations and an increase in other bacterial populations such as: Gardnerella spp, Prevotella spp, Bacteroides spp, Mobiluncus sp.
3. Condition III:
Bacterial vaginosis Positive (BVP) Is the complete loss of Lactobacilli population, presence of many other bacterial morphologies, especially the presence of Gardnerella vaginalis visible Clue cells (cells) vaginal epithelium on which is covered with small Gram-negative bacilli) in most cases.