This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
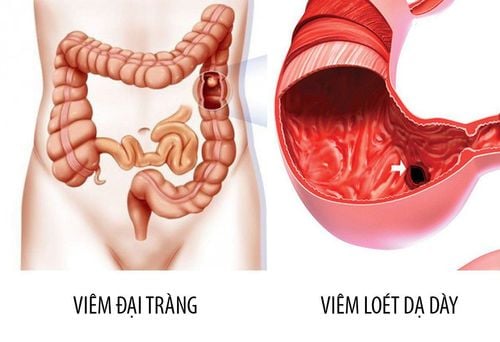
Hemorrhagic ulcerative colitis is a chronic inflammatory bowel disease affecting the colon with an unclear pathogenesis. The disease has manifestations outside the gastrointestinal tract such as skin lesions, purulent skin necrosis, joint damage, ...
1. Pathogenesis
Until now, although the pathogenesis of ulcerative colitis bleeding is not really clear, but the most mentioned hypothesis is that the pathological condition is caused by many factors that combine, including Genetics, environment, and gut microbiota affect inappropriate inflammatory responses.
2. Extra-gastrointestinal manifestations of ulcerative colitis bleeding
2.1. Skin damage
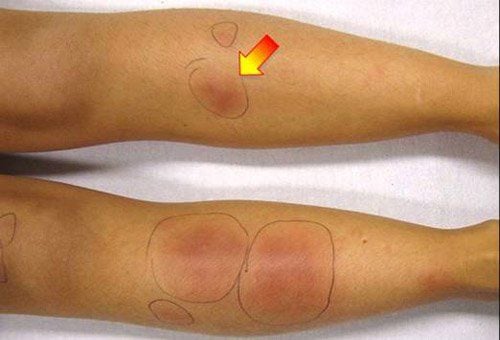
As in Crohn's, common skin lesions in hemorrhagic ulcerative colitis include erythema nodosum and pyoderma gangrenosum.2.1.1. Pink rash button
Erythema nodosum is a common skin lesion in inflammatory bowel disease, with an estimated prevalence of 15% in Crohn's disease and 10% in ulcerative colitis. The appearance of this skin lesion may be related to the level of inflammatory bowel disease activity.On the patient's skin, there are usually soft, congestive nodules, 1-5cm in size, bilaterally symmetrical in the knees, shins, ankles, rarely in the upper extremities. These nodules are usually non-ulcerative. In terms of progression, the nodules usually disappear after 2-6 weeks or so without scarring.
2.1.2. Purulent necrotizing inflammation of the skin
This is an uncommon skin disease characterized by polymorphonuclear leukocyte infiltration with widespread, rapidly progressive and painful ulcerative lesions. The estimated annual incidence is 3-10 million, of which 50% of patients have systemic diseases. About one-third of patients with this skin lesion have inflammatory bowel disease, of which ulcerative colitis is more common than Crohn's. There are many types of pyogenic gangrene including: typical, pustular, mucositis, blistering and superficial granulomatous. For patients with inflammatory bowel disease, the typical form often manifests as ulcers right around the stoma area or incisions that bring the bowel loops out of the skin. These lesions may persist from a few months to years and respond to topical corticosteroid treatment.
Skin pustular form is common in patients with active inflammatory bowel disease with separate, sterile pustules, usually 0.5 - 2cm in size with surrounding red halos. Patients often have additional symptoms such as fever and joint pain. The severity of skin lesions is related to the degree of inflammatory bowel disease activity. Therefore, when the intestinal disease is stabilized, the skin lesions also improve.
Mucosal purulent inflammation is quite rare but often occurs in patients with bleeding ulcerative colitis, characterized by pus-filled nodules in the mucous membranes of the mouth, nose, around the eyes, and vagina. When these pus-filled nodules burst, they will form erosions or ulcers.
Classification of types of pyoderma gangrenosum
| Mức độ | Đặc điểm |
| Điển hình | Các vết loét trên da với ranh giới không rõ, gây đau nhiều, thường thấy ở chi dưới. Ở bệnh nhân bệnh viêm ruột, có thể gặp tổn thương quanh vùng miệng nối đưa quai ruột ra ngoài da |
| Mụn mủ | Các nốt mụn mủ riêng biệt, vô trùng, bệnh nhân có thể kèm đau khớp, sốt. Có liên quan đến bệnh viêm ruột. Sự xuất hiện của tổn thương da liên quan đến mức độ nặng của bệnh lý nền |
| Viêm mủ niêm mạc | Tổn thương ở các niêm mạc, hay gặp trong viêm loét đại trực tràng chảy máu |
| Nốt phỏng rộp | Các nốt phỏng rộp, mụn nước gây đau. Ít gặp trong bệnh viêm ruột, hay gặp trong các bệnh máu ác tính |
| U hạt bề mặt | Tổn thương khu trú, thường không liên quan đến các bệnh lý khác |
2.2. Joint damage
25 - 40% of IBD patients have extra-gastrointestinal lesions, in which joint damage is quite diverse: 5 - 20% have peripheral arthritis; 1-26% have inflammatory lesions vertebrae and 24% of patients had sacroiliitis but no symptoms (detected on MRI). Although joint damage is more common in Crohn's, several community-based studies have reported that the prevalence of joint damage in patients with ulcerative colitis ranges from 15 to 21%.
Classification of joint damage in inflammatory bowel diseases has been mentioned in detail in the article Crohn's disease, including the main types: Spondyloarthritis, peripheral arthritis type, type II.
Type is characterized by a provincial-level lesion, affecting < 5 joints, including one large, bearing mainly. Type I is common in TBD patients who are in the active disease stage and have other manifestations outside the gastrointestinal tract (erythema nodosum, uveitis...).
Type II is common in multiple joints, regardless of the stage of inflammatory bowel disease. In a cross-sectional study with a relatively large sample size of 976 patients with ulcerative colitis with bleeding, the proportion of patients with peripheral joint damage type I was 3.6%, type II was 2.5. %. This rate is much lower than the results from the community because the exclusion criteria did not include patients with symptoms of musculoskeletal pain.
2.3. Eye damage
As in Crohn's, ocular lesions may occur in patients with ulcerative colitis with typical patterns including: episcleritis, scleritis, and uveitis. Rarely, optic neuritis or corneal vasculitis may occur.
Learn more about eye injuries, eye manifestations caused by bleeding ulcerative colitis in the following article.
MORE: Ocular manifestations of bleeding ulcerative colitis

2.4. Primary sclerosing cholangitis
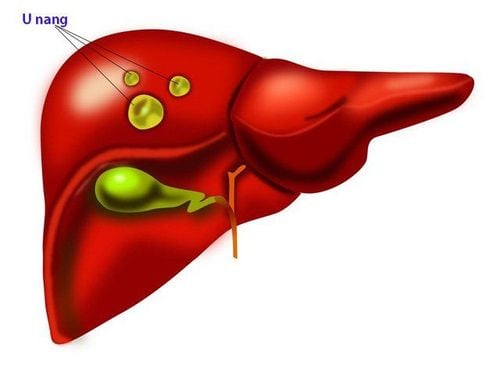
Primary sclerosing cholangitis is a chronic, progressive disease of the biliary tree characterized by fibrosis causing narrowing of the bile ducts, thereby leading to cirrhosis. In 1874, just 7 years after primary sclerosing cholangitis was defined, CH Thomas first mentioned the association between primary sclerosing cholangitis and hemorrhagic ulcerative colitis, when describing a case mortality with the presence of both diseases. In case cluster studies in Northern Europe and North America, the co-morbidity of inflammatory bowel disease in patients with primary sclerosing cholangitis ranged from 60 to 80%, of which ulcerative colitis was predominant. bleeding rate is about 85%. Inflammatory bowel disease is often diagnosed several years before primary sclerosing cholangitis, and especially in the group of patients treated with liver transplantation there is still an increased risk of developing inflammatory bowel disease. Therefore, all newly diagnosed cases of primary sclerosing cholangitis require colonoscopy and biopsy even in the absence of GI symptoms.
Several studies have documented that the progression of ulcerative colitis in bleeding in patients with primary sclerosing cholangitis tends to be more benign despite a higher incidence of total colonic involvement. In contrast, the rate of primary sclerosing cholangitis in the group of patients with inflammatory bowel disease does not have sufficient data to make a definitive diagnosis, patients should have cholangiography. The results of some studies show that an estimated 5% of patients with ulcerative colitis with bleeding co-exist with primary sclerosing cholangitis and during follow-up, the progression and severity of these two conditions may seems to be independent. The diagnosis of primary sclerosing cholangitis is based on clinical symptoms, laboratory tests, imaging features and liver biopsy.
2.5. Hematological Manifestations
2.5.1. Anemia
Anemia is common in inflammatory bowel disease, so in the recommendations, it is recommended to monitor hemoglobin every 6 months when the patient is stable and every 3 months if the patient is in the advanced stage. sick. Iron deficiency anemia or chronic disease is seen mainly in patients with ulcerative colitis with bleeding. Anemia due to vitamin B12 deficiency, folate less common; Anemia associated with the use of myelosuppressive agents should be considered in patients receiving sulfasalazine or thiopurine. Anemia due to autoimmune hemolytic or myeloproliferative disorders is rare.2.5.2. Formation of blood clots
In inflammatory bowel disease patients with multifactorial hypercoagulable state: Acute/chronic inflammation increases precursors of clotting factors (fibrinogen, factors V, VIII, IX), decreases anticoagulant factors clotting (protein C, S, antithrombin III), increased platelet aggregation... In addition, after surgery patients with limited mobility also contribute to an increased risk of venous thrombosis. One study found an 8.4-fold increased risk of venous thromboembolism in IBD patients within 120 days of a flare-up of gastrointestinal symptoms requiring steroid treatment.3. Progress
Progression of bleeding ulcerative colitis depends on the modality of treatment. In a community study, the median time patients had symptoms before, colectomy was during the first year. Without treatment, more than 90% of patients have recurrent episodes of persistent symptoms. Approximately one-third of patients with total ulcerative colitis require surgery as well as nearly 30% of patients on corticosteroid therapy who will require surgery within the next year. The mortality rate in this group of patients did not differ from the rate in the community.
Up to now, there is no specific medicine that completely cures bleeding ulcerative colitis. Only treatment can help limit the disease, reduce pain for the patient. Therefore, in addition to the treatment prescribed by the doctor, the patient needs to follow a good diet for the digestive system, avoid stress and need to have regular health checkups.
As soon as there are symptoms, it is necessary to go to the doctor soon for timely treatment when the damage has not spread. Vinmec International General Hospital with a team of highly qualified doctors, along with modern medical equipment and international standards, readers can trust to choose as a destination for examination and treatment. for yourself and your family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
The article references the source: NagreF, Gionchetti PR, Eliakim R., De Dombal F.T. (1968), Ulcerative colitis: definition, historical background, aetiology, diagnosis, naturel history and local complications, Postgrad Med, Crohn's B.B. (1962). An historic note on ulcerative colitis. Gastroenterology