This is an automatically translated article.
Posted by Doctor Nguyen Thi Hoai Nam - Department of Surgical Anesthesia, Vinmec Central Park International General HospitalEpidural anesthesia was once an effective method often considered the "gold standard" in the treatment of postoperative pain. However, recent evidence-based data have shown that the benefit of epidural anesthesia is not as significant as previously thought.
1. Is epidural anesthesia still the gold standard in postoperative pain relief?
Epidural anesthesia has some advantages in reducing the incidence of cardiovascular and respiratory complications, but these advantages may be limited to major thoracic or abdominal surgery in high-risk patients receiving external analgesia. simple dura mater. There is growing evidence that less invasive methods of pain relief are as effective as epidural analgesia.
Such methods include: Paravertebral anesthesia in thoracotomy; Fetal nerve block for total hip and knee replacement; Catheter incision in cesarean section, and local anesthetic technique in lower extremity joint replacement surgery.
Incisional anesthesia and its variants are simple and safe for other surgeries. Although epidural analgesia may be prominent, clinicians expect more from this highly experienced, expensive, invasive technique. Indications for epidural analgesia are declining for a number of different reasons. The decision whether or not to continue with the epidural should be guided by frequent monitoring and risk-benefit considerations more than before. For routine postoperative analgesia, epidural analgesia is no longer considered the gold standard.
Epidural analgesia is an effective technique in the treatment of postoperative pain that has been used for decades. Studies show that this technique has advantages such as reducing cardiovascular, respiratory and digestive complications and reducing mortality. This data combines national and international guidelines resulting in epidural analgesia being considered the gold standard in pain management after major surgery. Although epidural analgesia is invasive, experienced, and expensive; The costs and potential risks are considered reasonable because of the assumed benefits. Some studies suggest that shorter hospital stays when epidural analgesia is a factor in early recovery after major laparotomy, so cost-effectiveness adds to the benefits. However, it seems that the prevalence of epidurals is warranted for a number of reasons, including a more rigorous assessment of published data, and newer meta-analyses suggesting positive results. less, the acceptance of less invasive surgical techniques, the urgency of the strategy for early postoperative recovery, the widespread use of prophylactic anticoagulation, the availability of less invasive alternatives to regional analgesia than that are equally effective, the difficulty of implementing detailed controls in place provides risk-benefit data, and litigation concerns.
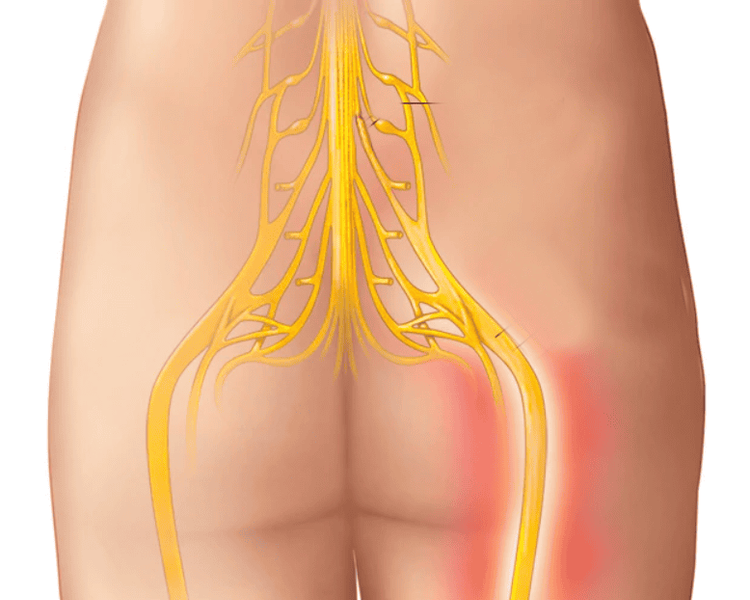
Gây tê thần kinh đùi trong các trường hợp thay khớp háng và khớp gối
2. Reduce epidural pain and mortality after surgery
Data from a meta-analysis from 141 randomized controlled trials (RCTs) that studied 9559 patients showed that epidural or spinal anesthesia was associated with a 30% reduction in 30-day mortality, Other advantages: 55% reduction in pulmonary embolism, 44% reduction in deep vein thrombosis, 50% reduction in blood transfusion requirements and 39% reduction in pneumonia. Evidence of other benefits such as reduced risk of respiratory failure, myocardial infarction, and renal failure.
However, a re-evaluation of this meta-analysis was found to be significantly flawed, and data from more recent meta-analyses and more rigorous studies in patients with aortic and gastric bypass surgery have been reported. , colonic and surgical procedures did not show a reduction in mortality with perioperative epidural analgesia compared with general anesthesia using systemic opioids. It is worthwhile to note that many published studies lack large enough sample sizes to evaluate rare outcomes such as mortality with an acceptable level of accuracy. With an estimated anesthetic-related mortality as low as 8.2 per million discharged patients, it was not possible to detect a difference in mortality in randomized controlled trials without present in millions of patients. Thus, there is no definitive and widely accepted evidence that epidural analgesia is associated with reduced perioperative mortality.
3. Cardiovascular complications
Animal and clinical studies suggest that thoracic epidural analgesia with local anesthetic can increase coronary blood flow and improve myocardial oxygen balance by affecting sympathetic nervous system activity. However, the benefit of epidural analgesia in reducing cardiovascular complications is not as clear as previously thought. The location of the epidural catheter seems to be very important. One meta-study found that thoracic epidural analgesia was more effective in reducing the risk of myocardial infarction than dorsal epidural analgesia.
Current evidence suggests that thoracic epidural analgesia may reduce the risk of cardiovascular complications such as myocardial infarction during major vascular surgery in high-risk patients. However, there is little evidence that epidural analgesia reduces cardiovascular complications in a relatively healthy, low-risk group. A meta-analysis of 28 studies involving more than 2,700 cardiac surgery patients found that epidural analgesia combined with general anesthesia was associated with a reduced incidence of supraventricular arrhythmias and respiratory complications but not mortality. heart attack or stroke. The authors concluded that the potential benefit of thoracic epidural analgesia was insignificant given the risks such as neuraxial hematoma.
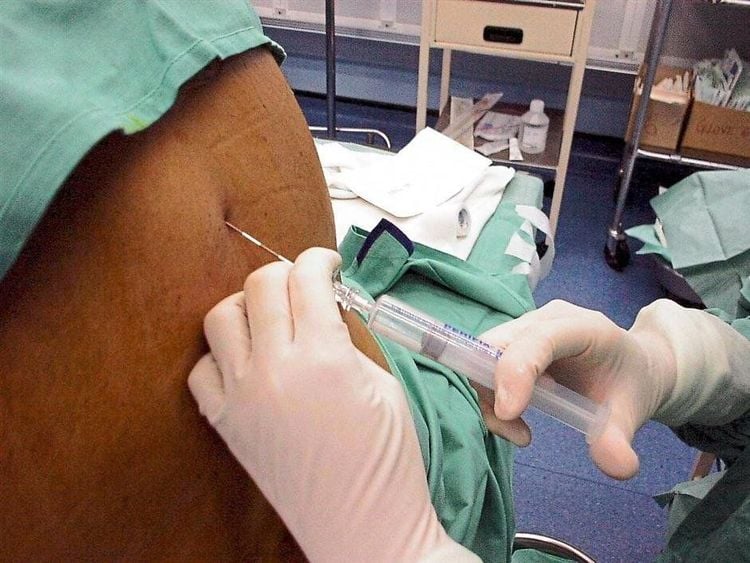
Hình ảnh giảm đau ngoài màng cứng đoạn ngực
4. Respiratory complications
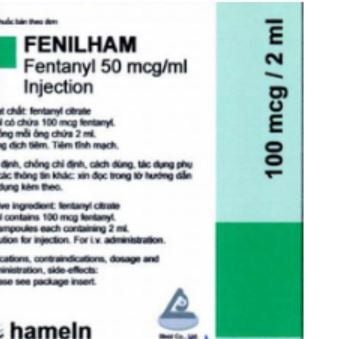
There is strong evidence that epidural analgesia is associated with a reduced risk of respiratory complications, particularly during open abdominal aortic or coronary bypass surgery. However, cardiovascular and gastrointestinal advantages are seen only when the epidural catheter is in the thoracic segment and only with non-opioid anesthetics. In clinical practice, epidural solutions often combine a low-dose local anesthetic with an opioid such as fentanyl. A meta-analysis of 50 RCTs showed that local anesthetic alone accounted for 4%, opioid alone 28%, and 68% combined anesthetic-opioid in the studies. In general, the protective effect against pneumonia of epidural analgesia after abdominal or thoracic surgery appears to have decreased over the past 35 years, probably due to the reduced risk of surgery. Controversy over the respiratory benefit of epidural analgesia is increasingly irrelevant as surgical techniques become less invasive.
5. Digestive complications
Significant adverse effects on the ileum after major abdominal surgery related to discomfort, complications, and prolonged hospital stay. Valuable evidence supports the view that epidurals, not opioids, can reduce the risk of ileostomy. A meta-analysis of 22 RCTs studying abdominal surgery showed that epidurals reduced the time to gastrointestinal recovery by 24-36 hours compared with systemic or epidural opioids. However, a meta-analysis of epidural analgesia after colorectal surgery showed that improved analgesia and reduced incidence of ileal complications did not shorten hospital stay.
A meta-analysis showed that continuous intravenous lidocaine infusion during and after surgery is a less invasive method associated with other advantages such as reduced ileal time, reduced pain scores, and decreased risk of postoperative vomiting and nausea surgery and reduced hospital stay. Chewing gum, an evidence-based approach to preventing or improving postoperative ileus is probably much simpler and safer.
There are currently no comparative studies showing that epidural analgesia reduces the risk of ileus more than intravenous lidocaine or chewing gum. In a recent paper, the authors state that there is a "serious lack of evidence to support the use of epidural analgesia and we question its routine use in postoperative analgesia." belly".

Giảm đau ngoài màng cứng có ảnh hưởng tới hồi tràng trong hệ tiêu hóa
6. Rate of thromboembolism
A meta-analysis reported in 2000 found that intraoperative neuraxial anesthesia reduces the incidence of deep vein thrombosis and pulmonary embolism. However, the majority of studies were performed prior to the advent of new thromboprophylaxis and minimally invasive surgery. The effect of postoperative epidural analgesia on coagulation regulation is unknown.
More recently, a meta-analysis of open aortic surgery, laparotomy, total hip and knee replacement did not demonstrate that epidural analgesia reduces thromboembolic complications. An overview of the influence of pathophysiological status, major surgery results noted that “In patients with gastrointestinal surgery without elective surgery, epidural analgesia did not seem to reduce anastomosis, blood loss in the anastomosis. surgery, need for blood transfusion, risk of embolism, cardiovascular complications, or length of hospital stay compared with conventional analgesia.
7. Patient satisfaction
In general, poor postoperative analgesia and analgesia side effects are associated with low patient satisfaction. However, patient satisfaction as an important goal is less studied. Only 2 RCTs out of 95 were recorded using a valuable tool to assess patient satisfaction. The authors note that “despite the hypothesized benefits of this superior analgesia, there is a lack of high-quality data on the efficacy of other analgesic modalities and regimens on patient outcomes reported such as health-related quality of life, quality of recovery and patient satisfaction.