This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Dinh Van Loc - Department of General Surgery - Vinmec Danang International General Hospital.
Endotracheal anesthesia is a technique of general anesthesia with endotracheal intubation for the purpose of respiratory control during surgery and postoperative resuscitation.
1. What is a liver abscess?
Liver abscess is the formation of pus in the liver, the pus can be large or small, solitary or many different pustules. Liver abscess is a dangerous disease because it can cause many serious complications. Liver abscesses can be caused by bacteria, parasites, or fungi. In developed countries, bacterial liver abscess is the leading cause, but worldwide, amoebic liver abscess is the most common cause.Most patients with bacterial liver abscesses and patients with amebic major liver abscesses are not reversible with antibiotics alone and need to be drained under ultrasound or CT guidance. Surgical drainage of an abscess is the process of draining pus out of an abscess to allow the lesion to heal faster. An abscess is a collection of pus located in your body. The cause of an abscess is usually an infection that has been attacked and destroyed by the body's immune system, leaving behind an abscess and pus called an abscess.
Liver abscess is a common disease in developing countries. Depending on liver damage, doctors will prescribe different treatment,
Its treatment has evolved over the past few years to day less invasive. Percutaneous drainage of the abscess is a well-established and perhaps most widely accepted method. However, large and multifocal abscesses containing thick pus may not be suitable for these methods.
– Need to aspirate the abscess to culture bacteria, aspirate pus or drain when the abscess is larger than 5 cm. If aspiration and drainage fail, perform surgery to drain.
In general, surgical drainage has been reserved for patients who have not responded to treatment with percutaneous drainage and antibiotics or who have concomitant intra-abdominal disease requiring surgical treatment. Therefore, percutaneous and surgical techniques are not competitive, but they have different indications and surgery also represents an option for those who do not respond to percutaneous therapy.
– If there is biliary obstruction, ensure biliary drainage by percutaneous drainage, stenting through retrograde cholangiopancreatography or surgery.
– Good control of blood sugar if you have diabetes.
– Treatment of primary bacterial foci if present in which the patient may require endotracheal anesthesia to surgically remove liver abscess.
2. Surgical treatment
Surgical drainage was considered the standard of treatment until the advent of percutaneous aspiration technique in 1970. With the aid of imaging guidance, percutaneous aspiration became the standard of care. treat.Indications for surgical management of pyogenic liver abscess are those associated with the patient's intra-abdominal condition such as peritonitis, the presence of abnormal intra-abdominal pathology such as management of diverticulitis, failure of previous drainage, presence of complications, multifocal abscess, wall thickening or thickening.
Laparotomy can be performed in two directions
A transperitoneal approach allows drainage of the abscess and probes the abdomen for signs of a previously undetected abscess and the location of the element epidemiology. For highly located posterior lesions, a retropleural approach may be used. Although this would be easier to access, it is not appropriate in cases of multiple lesions or where intra-abdominal specimens are difficult to obtain for pathology. An endoscopic approach is also commonly used in certain cases. This highly invasive technique allows visualization of the entire abdomen and significantly reduces mortality. Uncommon postoperative complications include recurrent pyogenic liver abscess, abdominal abscess, liver failure, renal failure, and surgical site infection.

Tới cơ sở y tế kiểm tra để phát hiện và điều trị áp xe gan kịp thời
3. Endotracheal anesthesia for liver abscess surgery?
Depending on the level of health status of the patient, the doctor will decide on the treatment, the use of anesthetic methods and the appropriate use of anesthetic drugs.May use drainage treatment and 2 to 3 antibiotics. Antibiotics are given intravenously until the fever and inflammation are gone. Or the doctor will appoint surgery for liver abscess with endotracheal anesthesia.
Endotracheal anesthesia for liver abscess surgery is a technique of general anesthesia, intubation with the aim of controlling the patient's breathing during surgery and postoperative resuscitation.
4. Procedure for endotracheal anesthesia for liver abscess surgery?
The patient was consulted with the anesthesiologist first, to assess the need for sedation before the day of surgery.4.1 Attention before anesthesia: In the meantime, broad-spectrum antibiotics should be used, if the patient is seriously ill, use antibiotics with strong effects and broad-spectrum activity like carbapenem immediately.
Assess the status of malnutrition and dehydration and electrolytes before surgery. Does the patient have septic shock? Complications of organs such as liver, kidney, Has the abscess burst into the lung? Good control of blood sugar if you have diabetes. 4.2 Position The patient is placed in supine position, breathing 100% oxygen 3-6 l/min before anesthesia for at least 5 minutes.
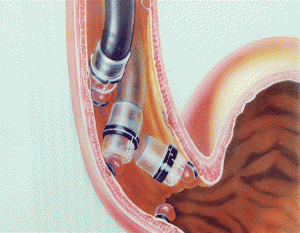
4.3 Endotracheal Anesthesia Technique Anesthesia technique has 2 techniques: Oral or nasal tube insertion.
Oral:
Open the mouth, insert the laryngoscope to the right side of the mouth, look for the epiglottis, orifice of the glottis. Rapid induction of anesthesia and a Sellick maneuver if stomach is full Insert endotracheal tube through the glottis Remove the laryngoscope gently. Endotracheal balloon pump. Check the correct position of the endotracheal tube with auscultation and EtCO2 results. Secure the tube with adhesive tape. Put the canul in the mouth to avoid biting the tube. Nasal route:
Anesthesia is given through the nose similar to the oral route, but before intubating the endotracheal tube, which is smaller than the oral route, a vasoconstrictor is instilled. Then insert an endotracheal tube lubricated with lidocaine ointment.

Kháng sinh được tiêm trực tiếp vào tĩnh mạch bệnh nhân
5. Notes after anesthesia surgery for liver abscess

Tùy phương pháp gây mê sẽ sử dụng ống nội khí quản phù hợp
After surgery, our patients always receive good analgesia care, prevent vomiting for patients at risk of nausea and vomiting after surgery, and have a heating system during and after surgery so most of the patients are very satisfied. heart, early mobilization, earlier recovery and discharge ...
Doctor Dinh Van Loc graduated as a General Doctor in Hue in 1990, graduated as a Specialist Doctor I in 2003 and a Specialist Doctor in Anesthesia II. resuscitation in 2017. Dr. Loc has advanced training in Anesthesiology and resuscitation and has more than 23 years of experience in pediatric intensive care anesthesia, cranial nerve anesthesia, and resuscitation anesthesia for patients. To register for examination and treatment at Vinmec International General Hospital, for detailed information and to schedule a medical examination and consultation, customers can call the hotline. hospitals or register for an online consultation with Vinmec International General Hospital HERE.