This is an automatically translated article.
Traumatic brain injury (TBI) has become a worldwide pandemic with more and more people being exposed as a result of the sequelae of contact sports, motor vehicle accidents or war.Long recognized as a potential cause of endocrine complications such as pituitary hormone deficiency (PHD), brain damage is also increasingly emerging as a research priority because In this context, pituitary hormone ratios, pathophysiological mechanisms, and responses to hormone replacement have not been clearly defined.
When thinking about the effects of brain damage (TBI) on the body, many people may immediately think of muscle weakness or spasticity, difficulty communicating, slow thinking.... Effects of traumatic brain injury. The brain on the body's endocrine system may be less obvious to the outside. However, endocrine dysfunction caused by brain damage can significantly affect a person's daily activities and is currently often overlooked or overlooked.
1. What is the endocrine system?
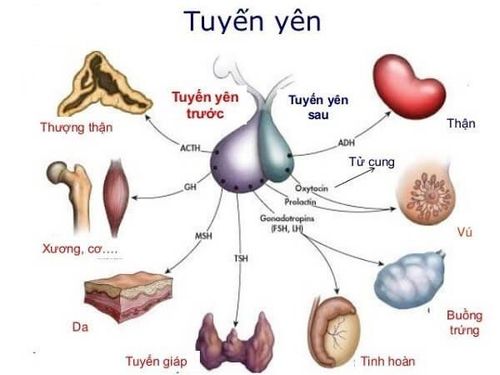
The endocrine system is a group of ductless glands that regulate biochemical processes and reactions in the body through the secretion of chemicals called hormones. The endocrine system is distributed throughout the body. These include the hypothalamus, pituitary gland, pineal gland, thyroid gland, parathyroid glands, pancreas, adrenal glands, testes, and ovaries. For the purposes of this article, the focus will be on the internal structures of the brain, hypothalamus, pituitary gland, and pineal gland.
Hệ nội tiết là một nhóm các tuyến không có ống điều chỉnh
2. How does the endocrine system work?
The hypothalamus is located in the ventral tegmental area of the brain. In simpler terms, it is located closer to the base of the brain. The hypothalamus is made up of a nucleus and subsections with distinct functional roles.
However, as a unit, the hypothalamus serves to regulate homeostasis, control the autonomic nervous system and visceral functions, and regulate appetite, temperature, thirst , stress response, lactation and respiratory function. It also has a role in the limbic system, an area of the brain that affects a person's emotions and behavior.
In addition to its role as a connection between the endocrine and nervous systems, the hypothalamus has functions in many regions of the brain. This demonstrates why the brain can function as a cohesive unit. For example, the hypothalamus receives information from the retina, cerebral cortex, amygdala, and hippocampus. Some of the areas where the hypothalamus sends information include the thalamus, brain stem, and pituitary gland.
The pituitary gland is approximately the size of a pea and is connected to the base of the hypothalamus. The pituitary gland can be divided into two parts; anterior lobes (in front of or toward the face) and posterior lobes (towards the back of the head).
The lobes have different roles and secrete different hormones. The anterior lobe regulates the thyroid, adrenal, and gonads. The anterior lobe is also the site of the production of growth hormone, prolactin, thyrotropin, and corticotropin. The function of the anterior lobe is regulated by the hypothalamus. The posterior lobe of the pituitary gland, which is an extension of the hypothalamus, secretes two hormones produced in the hypothalamus; vasopressin (also known as antidiuretic hormone or ADH hormone) and oxytocin. The pituitary gland also secretes endorphins, a hormone that acts on the nervous system and reduces pain and menstrual cycles in women.
Also located in the brain, the pineal gland or pineal gland produces melatonin which helps regulate each person's circadian rhythms. The circadian rhythm is the internal clock that regulates biological and behavioral processes.
Hormones produced and secreted throughout the endocrine system travel through the bloodstream to affect specific organs. Excessive or low secretion of hormones, or the inability to effectively utilize hormone targets, leads to a state of endocrine dysfunction.
3. Brain damage and endocrine dysfunction
Brain injuries are the effects of concussions in the head region on the brain. Traumatic brain injury includes two types:
Primary injuries are local injuries, such as bleeding, and diffuse longitudinal injuries, such as tension, tear, and ablation. Secondary injuries of traumatic brain injury include swelling, decreased oxygen levels, increased cranial pressure, and nerve damage. Injury to the hypothalamus and pituitary gland may develop after a patient has suffered a traumatic brain injury. These structural changes may include damage to the pituitary-hypothalamic stalk, anterior lobe necrosis, and posterior lobe hemorrhage. In the anterior lobe of the pituitary gland, damage is typically due to infarction. Swelling can also cause injury due to the relatively tight space in which the pituitary gland resides. Posterior lobe lesions are most commonly caused by acute bleeding. These types of injuries are not uncommon. One study found that during autopsies, up to a third of fatal traumatic brain injuries involved pituitary necrosis. In addition, another study demonstrated that hypothalamic damage was common after traumatic brain injury, occurring in 42% of brain injuries that resulted in death.
Neuroendocrine conditions commonly seen after traumatic brain injury include syndrome of inappropriate antidiuretic hormone secretion (SIADH), diabetes insipidus, and anterior pituitary insufficiency.
Diabetes insipidus is caused by antidiuretic hormone (ADH) not being released due to damage to the posterior pituitary gland. The most common symptoms are thirst and dilute urination. Antidiuretic hormone causes blood thinning and hyponatremia secondary to too much antidiuretic hormone. Symptoms include fatigue, weakness, muscle cramps, decreased appetite, increased thirst, nausea/vomiting, seizures, confusion, and changes in urination habits. Symptoms of hypopituitarism characterize this hormone deficiency. People with this condition may initially have no symptoms.
4. Neuroendocrine dysfunction after brain injury
The prevalence of pituitary dysfunction in traumatic brain injury survivors is estimated to be 37-59%. Other statistics on hormonal abnormalities are even higher.
In some studies, the suggested rate of dysfunction depends on the severity of the injury. The dysfunction may be more severe in people with more severe injuries. However, several other studies have not shown a clear relationship between injury severity (as measured by the Glasgow Coma Scale) and the presence of pituitary dysfunction. The variable hormone deficiency rates were found immediately after injury and 12 months after injury with growth hormone deficiency being the most common deficiency (37.7% of cases one year after traumatic brain injury). Brain).
Tỷ lệ rối loạn chức năng tuyến yên ở những người sống sót sau chấn thương sọ não được ước tính rơi vào khoảng 37-59%
5. Neuroendocrine dysfunction and daily functioning
Neuroendocrine dysfunction can aggravate physical and neuropsychiatric conditions following traumatic brain injury. Symptoms of neuroendocrine dysfunction are similar to those after brain damage. These include: depression, anxiety, fatigue, poor memory, difficulty concentrating, decreased sex drive, infertility, missed periods in women, weight gain or loss, increased fatty tissue around the abdomen, lower blood pressure , decreased heart rate, anemia, constipation, dry skin.... However, many people tend to overlook endocrine dysfunction and focus only on traumatic brain injuries.
Fortunately, there are methods used to evaluate endocrine dysfunction, including neuroimaging that can help visualize hypothalamic or pituitary damage. Blood tests may be used to evaluate hormone levels. Sensitive assessment of hormone levels in the post-acute period is recommended by many experts.
Specifically, assessment of pituitary function and growth hormone reserves is recommended for all survivors of moderate to severe traumatic brain injury one year after injury. Endocrinologists familiar with traumatic brain injury can provide useful information to facilitate recognition of deficiency and ensure appropriate treatment. As part of the traumatic brain injury team, an endocrinologist may prescribe medications and prescribe hormone replacement therapy to address endocrine dysfunction caused by traumatic brain injury.
In summary, endocrine dysfunction is common after traumatic brain injury. Because many of the signs of hormone deficiency are similar to cognitive and behavioral symptoms after a traumatic brain injury, endocrine dysfunction can be easily overlooked. Because many of these deficiencies can be medically resolved, it is important to work with a physician to evaluate and treat endocrine dysfunction when appropriate.
The biggest challenge for endocrine complications in patients with traumatic brain injury is making an early assessment of these disturbances. Endocrine complications can significantly influence the progression and outcome of traumatic brain injury. The release of pituitary hormones, controlled by nerve signals from the hypothalamus, provides tight control of hormone homeostasis. The pituitary gland is protected in the pituitary fossa of the sphenoid bone.
However, the pituitary stalk, which connects the anterior pituitary and the hypothalamus, is susceptible to traumatic brain injury, especially in patients with facial fractures, skull base fractures, and cranial nerve damage. .
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: rainbowrehab.com