This is an automatically translated article.
Article written by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Liver cells act as a storehouse of many important substances such as iron, vitamins, minerals, ... until the body needs to use them. Patients with cirrhosis have the highest mortality rate only after liver cancer, which is the ultimate consequence of chronic liver disease. In it, the damaged cells are replaced with fibrous, scarred and proliferative nodules, over time, the liver will gradually lose its ability to repair itself and function normally.
1. Overview of current cirrhosis of the liver
With the rise of metabolic syndrome and obesity globally, metabolic-associated fatty liver disease (MAFLD) has been recognized as the most common cause of chronic liver disease in the United States. Globally, the disease has an increasing impact, with it estimated that cases of MAFLD will increase from 83.1 million in 2015 to 100.8 million in 2030 in the United States alone. Chronic liver disease and cirrhosis have a major impact on the health care system and remain a public health concern.
Currently, there are no anti-fibrotic therapies approved by the Food and Drug Administration for clinical use. However, with an improved understanding of the underlying cellular and molecular mechanisms underlying cirrhosis, scientists and clinicians can continue to develop therapeutic targets that can inhibit, change or even reverse liver fibrosis.
2. Pathophysiology of liver fibrinogenesis
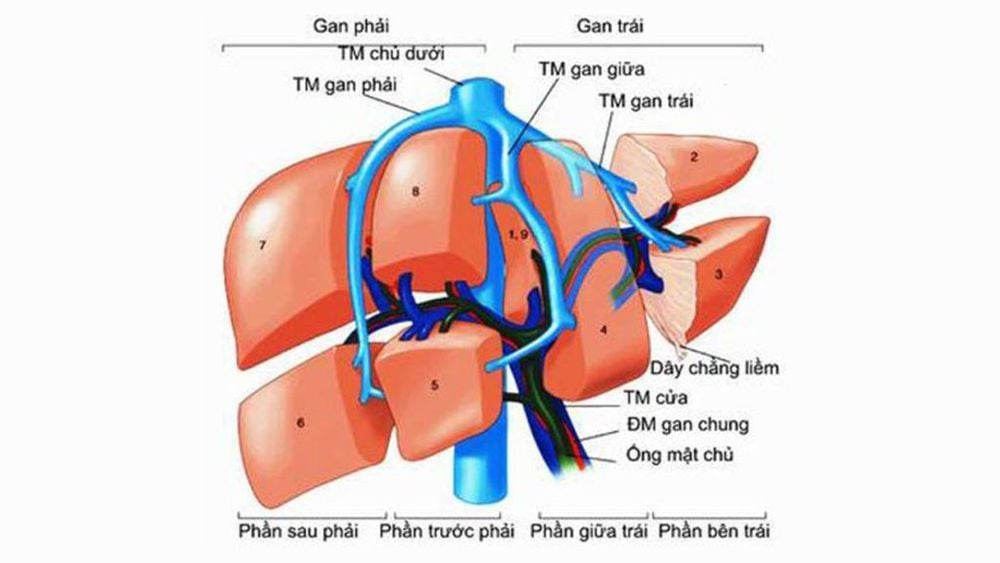
The liver is composed of parenchymal cells (i.e. hepatocytes) and non-parenchymal cells. Hepatocytes arranged in lobules account for 60%-80% of the total liver mass, with the portal triad (hepatic artery, hepatic portal vein, bile duct) and central vein (Kupffer's cell) being macrophages. Specialized cells reside in the lumen of the hepatic sinusoids, playing an important role in initiating the immune response.
Liver sinusoidal endothelial cells form a sinusoidal (endothelial) pattern, forming a fenestrae that allows filtration of a wide variety of solutes and particles between the blood entering the sinusoidal lumen and hepatocytes. Liver astrocytes (Astrocytes) are resident mesenchymal cells found in the endothelial space of Disse. After exposure to inflammatory cytokines, chemokines and other noxious stimuli; quiescent astrocytes transform into proliferative, migratory, and contractile fibroblasts (activated state). These in turn produce components of the extracellular matrix (a major factor in liver fibrosis).
Gan được cấu tạo bởi các tế bào nhu mô (tức là tế bào gan) và các tế bào không nhu mô.
3. Disease-specific targeted therapies
3.1. Alcoholic liver disease
The importance of abstaining from alcohol has been shown to benefit survival in people with alcoholic liver disease. It has been reported that abstaining from alcohol leads to a statistically significant improvement in 5-year survival of 75% compared with 50% in those who continue to drink. However, histological data were not collected. A rapid decline in liver stiffness with the use of FibroScan ® TE was demonstrated in one study: 1 week of abstinence resulted in a decrease in hepatic stiffness in 45% and an estimated reduction in fibrosis stage in 23% of patients abstinence.
Continued transient decrease in elastography was observed in another study that showed a significant decrease in TE in patients day 8 (41.7%) and day 60 post-abstinence (66.7%). Candesartan, an angiotensin II type 1 receptor blocker, has also been shown to significantly reduce fibrosis scores, fibrosis area, and smooth muscle actin when used in combination with ursodeoxycholic acid (UDCA) compared with with UDCA alone in alcoholic patients.

Candesartan, một chất ngăn chặn thụ thể angiotensin II loại 1, cũng đã được chứng minh là làm giảm đáng kể điểm số xơ hóa.
3.2. Autoimmune hepatitis
The mainstay of treatment in autoimmune hepatitis (AIH) is to reduce inflammation through the use of high-dose corticosteroids alone or in combination with immunomodulators such as azathioprine, which may ultimately stop the progression of the disease. fibrosis in the liver. In one study, 53% of AIH patients treated with corticosteroids demonstrated improved fibrosis scores (Ishak score), as well as a reduction in the frequency of histologically demonstrated cirrhosis from 14 patients. (16%) at treatment initiation down to 10 patients (11%) during the 63-month treatment period.
Similar improvements were demonstrated in a group of 19 patients treated with cyclosporine A with prednisolone for 6 months; thereafter, continue maintenance therapy with azathioprine. Paired liver biopsies both before and after treatment showed significant improvement in the mean fibrosis stage and inflammation level. A more recent study confirms the effectiveness of immunosuppression in promoting biochemical remission along with resolution of fibrosis. It even improved near-normal liver histology after prolonged AIH treatment.
It is thought that corticosteroid therapy allows histological improvement through both direct and indirect effects - fibroblasts; inhibit the transformation of astrocytes into fibroblasts, reduce liver inflammation; ultimately interfere with the molecular signals of fibrosis and facilitate extracellular matrix degradation.

Trong một nghiên cứu, 53% bệnh nhân AIH được điều trị bằng corticosteroid đã chứng minh được điểm số xơ hóa được cải thiện.
3.3. Nonalcoholic fatty liver disease/metabolic-associated fatty liver disease
MAFLD also known as non-alcoholic fatty liver disease (NAFLD) has become the most common cause of chronic liver disease in the West. However, optimal therapy has not yet been discovered and is currently based on identification of risk factors with dietary and lifestyle modifications.
Many studies have shown a positive effect of weight loss in improving MAFLD and preventing the progression of non-alcoholic steatohepatitis (NASH)/cirrhosis. 5% weight loss through calorie restriction has been shown to improve adiposity; 5% to 7% weight loss can improve inflammation; 7% - 10% weight loss leads to NAFLD/NASH remission and improved fibrosis Hohenester et al.'s investigation showed that 11.8% of patients demonstrated liver fibrosis at baseline through fibrosis score. NAFLD. After weight loss, 0% of patients developed fibrosis at 52 weeks (P < 0.05).
However, an earlier randomized controlled trial with a mean weight loss of 9.3% did not confirm a significant change in liver fibrosis. Despite improvement in NASH histological activity scores in 31 patients over 48 weeks. Several studies have shown histological improvement, including reduction in fibrosis after spondylectomy. A meta-analysis of pre- and postoperative histological findings demonstrated a mean reduction in fibrosis rate of 11.9% (P<0.0001) in obese patients with MAFLD undergoing laminectomy. Similar findings were found in a systematic review and meta-analysis performed by Mummadi et al. Of these, 65.5% of patients showed improvement or resolution of fibrosis after weight loss due to end-stage surgery.
Role of Vitamin E and pioglitazone in the treatment of nonalcoholic steatohepatitis (NASH) The results of the PIVENS trial have led to the current AASLD recommendations for the use of Vitamin E (800 IU/day) or pioglitazone for the treatment of NASH in non-diabetic patients. This trial was a large randomized controlled trial of vitamin E versus pioglitazone and placebo, in which 247 adults with non-diabetic NASH (biopsy confirmed) were assigned to one of two treatment groups. .
Use of both drugs was associated with significant reductions in steatosis, lobular inflammation, and liver enzymes compared with placebo; however, there was no reduction in liver fibrosis. It is important to exercise caution when prescribing these drugs because there are data showing increased rates of prostate cancer and mortality with the use of Vitamin E. Common side effects are weight gain and loss. Bone also needs to be considered when prescribing thiazolidinediones, such as pioglitazone.
Role of fibroblast growth factor (FGF) Other areas of investigation for fibroblast therapy in NASH include fibroblast growth factor (FGF). FGF19 is a polytrophic protein that has been shown to decrease gluconeogenesis and increase insulin sensitivity, inhibit fatty acid synthesis, increase hepatic glycogen and protein synthesis, and regulate bile acid homeostasis. In a recent phase 2 study, Aldafermin (NGM282), an FGF19 analog, demonstrated histological improvement in patients with NASH.
After 12 weeks of treatment, paired liver biopsies showed a decrease in NAFLD activity score (NASH) in both the 1mg and 3mg treatment groups (P<0.001), as well as a decrease in fibrosis score in 3 mg group (P = 0.035). Results also demonstrated NASH improvement of 2 points or more without fibrosis in 50% and 63% of patients in the 1mg and 3mg treatment groups, respectively (NCT02443116). In phase 2 test; The authors noted gastrointestinal side effects including nausea, abdominal pain, diarrhea and injection site reactions following administration of NGM282. FGF21 is similar, as it plays multiple roles in metabolism, including fatty acid oxidation, lipolysis, and gluconeogenesis.
Role of the drug Pegbelfermin Pegbelfermin (BMS-986036) is a pegylated human FGF21 analog. It showed a significant reduction in the absolute percentage of liver fat in the 10mg daily group (-6.8% vs -1.3%; P=0.0004) and in the weekly 20mg subgroup (-5.2% vs -1) .3%; P = 0.008) compared with placebo in patients with NASH fibrosis stage 1 - 3 (NCT02413372). Common side effects of drug treatment include diarrhea and mild nausea.

Nhiều nghiên cứu đã chỉ ra tác động tích cực của việc giảm cân trong việc cải thiện gan nhiễm mỡ không do rượu.
4. Conclusion
The formation of liver fibrosis and progression to cirrhosis is a complex mechanism that interacts between the formation of the fibrous matrix and its degradation. There are many causes of fibrosis and cirrhosis of the liver. While most trials currently focus on MAFLD, further research is needed among all causes of cirrhosis to improve benefit worldwide.Currently, in order to improve service quality, as well as create more conveniences for patients, Vinmec deploys a comprehensive Hepatobiliary Screening Package to help diagnose cirrhosis in particular and hepatobiliary diseases in general. for all customers. Vinmec is the leading prestigious and reliable address in the field of screening and treatment of hepatobiliary diseases, with the following advantages:
Possessing modern facilities, full of advanced equipment and machinery world leading, for high image quality, accurate and fast test results, maximum support for disease diagnosis and treatment. A team of leading specialists from major hospitals across the country helps the treatment process to be highly effective and shorten the treatment time. Professional and comprehensive examination and consulting services, examination space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Abbreviations:Astrocytes (HSCs)
Chronic hepatitis B (CHB)
Autoimmune hepatitis (AIH)
Nonalcoholic steatohepatitis (NASH)