This is an automatically translated article.
Posted by Resident Doctor, Master Tran Duc Tuan - Department of Diagnostic Imaging - Vinmec Central Park International General Hospital
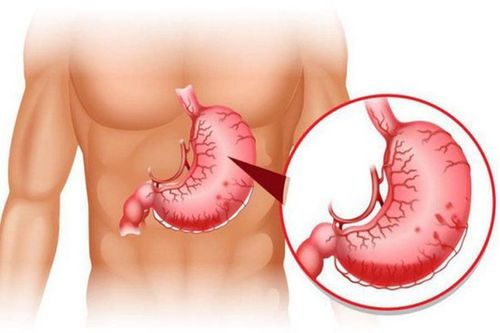
Increased pressure in the portal vein due to cirrhosis can cause serious complications such as gastrointestinal bleeding due to rupture of esophageal and gastric varices. . Digital subtraction angiography and percutaneous portal shunts (TIPS) are very effective treatments for the prevention of complications of portal hypertension in cirrhosis.
1. What is digitized background removal and percutaneous access (TIPS)?
Transjugular Intrahepatic Portosystemic Shunt (TIPS) or percutaneous transluminal catheterization has been performed since the 1980s to treat some complications of portal hypertension. The principle of TIPS is to create an anastomosis, between a hepatic vein and a venous tributary, by means of a passage through the liver. The aim is to reduce pressure in the splenic, superior mesenteric, and portal venous systems in portal hypertension.
Digital Subtraction Angiography (DSA) is a new vascular imaging technique by X-ray. This is an imaging method that combines X-ray and digital processing using algorithms. to remove the background on the 2 images obtained before and after the contrast agent was injected into the patient's body. The purpose of this technique is to study blood vessels in the body and see more clearly the lesions and vascular pathology before vascular intervention is indicated.

2. Specify digital capture to remove the background and create a portal through the skin
The method is indicated for patients who have failed sclerotherapy of esophageal varices (considered immediate failure or recurrent bleeding after two sclerotherapy within 15 days) Other bleeding causes related to portal hypertension: gastric bleeding due to varices in the stomach or other sites such as duodenum, colon... Recurrent ascites (abdominal effusion but not Treatment with conventional methods is not effective) Budd-Chiari syndrome Relatively rare indication: Place TIPS before endoscopic or surgical treatment in patients with esophageal tumors with varicose veins.
3. Contraindications for digitizing background removal and percutaneous ossification
Absolute contraindications for: Severe right-sided heart failure that can cause acute heart failure on the background of chronic heart failure after portal flow Severe pulmonary arterial pressure (pulmonary artery pressure > 45 mm Hg) Severe liver disease Relative contraindications: There is usually no indication for percutaneous porto-portal catheterization: Concurrent liver tumors are not indicated, but depend on the size, location and treatment strategy (liver transplantation, radio frequence.. .) Partial or complete portal vein thrombosis, this is not an absolute contraindication. However, as a possible factor for procedure failure, it is necessary to assess whether the thrombus is old or new, whether it can be perforated or not, and the location of the thrombus. Incomplete thrombosis is not a contraindication, but it is a factor in procedural difficulty. Be careful with pregnant women. Polycystic liver is also a complicating factor in the procedure.
4. Advantages of the method
The method of creating a percutaneous portal shunt is an endovascular interventional method, which is less invasive as well as helps to reduce complications compared to other methods, increasing the possibility of recovery after the intervention. This is a method that can prevent gastrointestinal bleeding or emergency treatment of gastrointestinal bleeding caused by rupture of varicose veins of the esophagus and stomach that are not effective by medical or endoscopic treatment, ie. Patients who have had esophageal varices many times but still have recurrent bleeding or in some cases can not be treated with endoscopic venous ligation.
5. Steps to take
5.1 Before the procedure
The decision to perform percutaneous transhepatic porto-hepatic shunt should be consulted by radiology and hepatobiliary specialists, and endoscopically for a specific strategy. Patients are assigned to perform general tests of liver function, kidney function, bleeding-clotting, 3-phase computed tomography of the liver or magnetic resonance imaging to evaluate liver morphology, resolution changes. Liver vein surgery, portal vein system, draining veins, hepatic artery and liver tumor detection, echocardiography to evaluate cardiac function. In the case of an emergency (gastrointestinal bleeding) only a Doppler ultrasound is needed. Before the procedure, the patient is clearly explained about the procedure, and should fast for 6 hours before the procedure.

5.2 Steps to take
Anesthesia: general anaesthesia Opening the lumen: Insert the needle into the internal jugular vein. Insert the catheter into the internal jugular vein. Angiography: inserting a catheter into the suprahepatic vein, taking a portal vein by injecting contrast material from the superior hepatic vein through the liver parenchyma into the vein. Creating a portal-host bridge: Insert the barrel of the ROSS needle into the superior hepatic vein. Aspiration from the superior hepatic vein into the portal vein is considered the most difficult step of the procedure. After syringe contrast imaging shows that the ROSS needle is in the portal venous system, push the lead through the iron barrel and attempt to push down the superior mesenteric or splenic vein. Expand the tunnel with a balloon on a rigid conductor. Measure the pressure difference between the anterior and posterior portal veins of the liver. Place a luminal support (rack frame) from the superior hepatic vein into the portal vein. Re-measure the portal venous pressure difference before and after the liver, compare with the pressure difference before placing the Bracket to evaluate the effectiveness.

6. Complications can be encountered during percutaneous transhepatic porto-hepatic shunt intervention
6.1 Complications related to the intervention process
The procedure may fail when the jugular vein cannot be punctured Acute renal failure in pre-interventional patients with limited renal function. Piercing the liver capsule and causing damage to the liver parenchyma is a common complication (about 10%) A portal vein shunt with the hepatic artery can be encountered, if the flow is large, it may be possible to occlude the catheter with a spiral needle. arterial type. Communication between the scaffold (supporting frame) and the biliary tree, this complication can cause jaundice and infection. If medical treatment is not effective, it may be necessary to block the catheter and create a new one. Bile duct bleeding. When the needle penetrates the liver, it is possible to injure the hepatic artery or the gastroduodenal artery causing intra-abdominal bleeding, or pseudoaneurysm, which can be treated with percutaneous endovascular intervention. arteries or surgery. Movement of the metal support can cause atrial perforation and acute pulmonary edema. This is a rare complication Infection, a complication is very common, especially in patients with cirrhosis, clinical manifestations are fever, hepatomegaly, positive blood cultures and sometimes thrombosis in the lumen of the rack. Antibiotic treatment may be effective for these clots.

6.2 Late complications
Narrowing or occlusion of the bracket: To detect this complication, it is necessary to have Doppler ultrasound of the catheter, usually 24 hours after the intervention, 1 week, 1 month, then regularly every 3-4 months. Hepatobiliary syndrome: This complication may occur in 20-30% of cases of percutaneous portal opening. Digital background erasure and percutaneous transluminal angiography is an imaging technique that requires a high level of experience by the physician and the perfect coordination of the patient. In order to achieve high diagnostic efficiency, patients need to choose reputable addresses that have digital scanning machines to erase the background and have modern and standard medical equipment from which to have timely treatment.
Vinmec International General Hospital is a hospital with a full convergence of general and specialized doctors to perform, examine, operate, diagnose and treat diseases. In particular, at Vinmec, the technique of digital imaging to remove the background is also performed to diagnose images, thereby offering treatment plans for many different diseases and providing optimal treatment results for customers.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.