This is an automatically translated article.
This article is professionally consulted by Master, Doctor Vu Huy Hoang - Radiologist - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International Hospital. Doctor Vu Huy Hoang has 10 years of experience working in the field of diagnostic imaging.Digital erasure angiography (DSA) and catheter thrombectomy are performed by inserting a suitable diameter catheter to the site of the thrombus, followed by negative pressure aspiration to remove the thrombus. blood clot.
1. What is acute arterial thrombosis of the extremities?
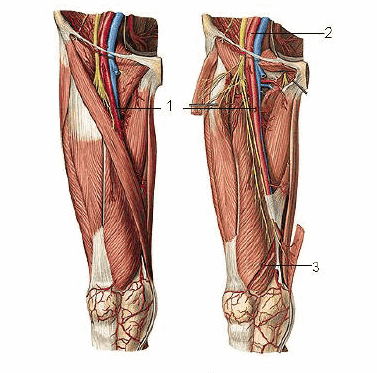
Acute limb artery thrombosis is a condition in which the artery supplying the limb is occluded, causing acute limb ischemia, affecting the ability to preserve the limb. This is a cardiovascular surgical emergency, resulting in acute ischemia of the limb that the artery nourishes. If the acute extremity thrombus is not removed quickly, the limb with ischemia will become necrotic.Causes of acute arterial thrombosis of extremities include:
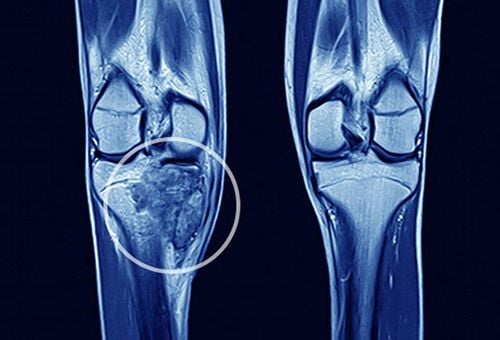
Vascular trauma: This is the most common cause of acute arterial thrombosis. This is more common in patients with vascular trauma to the arteries and may be accompanied by long-bone fractures in the extremities. Injuries due to arterial procedures: X-ray angiography, cardiac catheterization, percutaneous transluminal angioplasty. Blood clots on ulcers of atherosclerotic plaque: Arterial clot formation also accounts for a significant proportion of acute arterial thrombosis of the extremities. Signs of arterial occlusion due to acute arterial thrombosis of the extremities:
Changes in skin color in the extremities: When the limb arteries are blocked, the skin in the ischemic extremities becomes pale, with scattered purple spots. waste due to hemorrhagic necrosis in the area of tissue ischemia. Severe pain: Pain often occurs suddenly in the limb that has an embolism. Numbness: Patients often have a feeling of numbness and tingling. At first, there will be a superficial feeling on the skin, then the patient will lose the feeling of depth. Cold extremities: In the area of the limb with arterial occlusion due to thrombosis, the extremity is usually colder than the unaffected side. Loss of pulse below the occluded artery: This is the objective sign to identify acute thrombotic limb artery occlusion. Signs of muscle paralysis: Usually after an artery is blocked, the ischemic muscles will have reduced function, the movement of the fingers in the limb with the artery is weaker and then completely paralyzed.
2. Treatment of acute arterial thrombosis of extremities

However, catheter thrombectomy (DSA) for acute extremity thrombosis is the optimal approach.
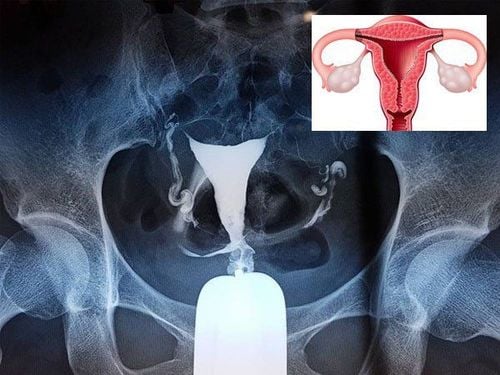
The catheter thrombectomy DSA is performed by inserting a suitable diameter catheter to the site of the thrombus, then performing negative pressure aspiration to remove the thrombus.
2.1. Indications and contraindications Indications for implementation:
Acute venous thromboembolism of the extremities < 3 weeks Thrombo length not more than 3 cm Contraindications for performance:
Chronic venous thromboembolism of the extremities > 3 weeks The clot is more than 3cm long. Allergy to iodinated contrast agents Grade IV renal failure Coagulation disorders and loss of control Pregnant women. 2.2. Step 1: Prepare a DSA scanner, a dedicated electric pump, an image storage system, an X-ray shield; anesthetics, anesthetics, anticoagulants, neutralizing anticoagulants and water-soluble iodine contrast agents; antiseptic solution for skin and mucous membranes; specialized medical supplies; occlusive materials. Step 2: Ask the patient to lie on his back, install a monitor to monitor breathing, pulse, blood pressure, electrocardiogram, SpO2, then disinfect the skin and cover with a sterile cloth with holes. Step 3: Anesthesia: The patient lies supine on the scanning table and intravenous line is placed and local anesthetic is applied. Step 4: Arterial puncture: Most femoral artery puncture, can be retrograde or downstream. In special cases, a puncture from the brachial artery can be performed. Step 5: Arterial DSA and selective threading of the injured artery. After that, identify the damaged blood vessel, then insert the catheter with suitable diameter to the clot site, conduct negative pressure suction to remove the thrombus. It can be done several times until the thrombosis is gone.
3. Monitoring and handling of accidents

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
MORE
Lower extremity atherosclerosis: Signs and treatment Lower extremity artery disease: How is it treated? Beware of lower extremity peripheral artery occlusion