Gastritis and Irritable Bowel Syndrome (IBS) are two common gastrointestinal disorders, especially prevalent among those with modern lifestyles. Although they both cause abdominal discomfort, these conditions have distinct characteristics. Let's explore the differences in their causes, diagnosis, and treatment.
This article is written with the professional guidance of doctors from the Gastroenterology and Hepatology Department at Vinmec International General Hospital.
1. What are gastritis and Irritable Bowel Syndrome?
Before exploring the differences and similarities between gastritis and Irritable Bowel Syndrome (IBS), it is important to understand the definitions of these two conditions.
1.1. Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a disorder affecting the function of the digestive system, primarily occurring in the large intestine (colon), and is also known as spastic colon.
IBS is a chronic disorder characterized by recurrent digestive symptoms without any physical damage or structural changes in the colon. The factors causing this condition include:
- Psychological Factors: anxiety, excessive thinking, prolonged stress,...
- Neurological issues like depression, insomnia, or sleep disorders.
- Diet: Poor eating habits, consumption of toxic foods, or spoiled food…
- Other Causes:
- A history of intestinal diseases.
- Women during menstruation.
- Use of hormonal medications or related endocrine disorders.
- Genetic factors…
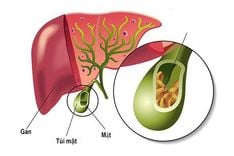
1.2. Gastritis
Gastritis is a condition where the stomach lining is physically damaged due to inflammation. This damage can penetrate the muscular layer of the stomach lining. Gastritis is categorized into two main types: acute and chronic, with chronic being more commonly seen in clinical practice. The causes of these conditions include:
Bacterial causes:
- The most common cause is infection with Helicobacter pylori (HP).
- Possible infection with Helicobacter heilmannii.
- Other bacteria such as Mycobacterium, Histoplasmosis, or Syphilis.
- Parasitic infections, such as threadworms...
- Viral infections like Cytomegalovirus (CMV) or Herpes
Non-bacterial causes:
- Autoimmune diseases or allergies.
- Use of non-steroidal anti-inflammatory drugs (NSAIDs), aspirin, or certain antibiotics.
- Abuse of alcohol, tobacco, and coffee.
- Poor dietary habits, such as irregular meals, late-night eating, skipping meals, or consuming spicy foods.
- Unhealthy lifestyle habits, like staying up late.
- Psychological factors or autonomic nervous system disorders.

2. Clinical symptoms
2.1. Irritable Bowel Syndrome
Chronic intestinal disorders manifest through recurrent abdominal pain, occurring at least once a week for at least the past three months, along with two or three of the following factors:
- Associated with bowel movements.
- Changes in the frequency of bowel movements.
- Changes in the appearance of stool.
Accompanying signs include:
- Frequent abdominal pain and discomfort after eating or during stress.
- Changes in bowel habits.
- Constipation or diarrhea, which can occur alternately or individually.
- Bloating.
2.2. Gastritis
- The pain may occur in the epigastric region or the area above the navel. The pain is often dull but can sometimes become very intense, accompanied by a burning sensation and discomfort. The pain typically increases when eating or immediately after a meal, especially when consuming alcoholic beverages or spicy, sour foods.
- Bloating and distension.
- The patient may feel nauseous or vomit frequently after eating and may feel relief after vomiting. In some cases, the patient may vomit sour fluid or blood if there is no food left in the stomach.
- Other symptoms include loss of appetite, a bitter taste in the mouth, bad breath, lack of enjoyment in eating, and indigestion.
- Patients may also experience digestive disorders such as diarrhea or constipation.
- In cases of acute gastritis, the patient may have a mild to high fever.
- A gnawing sensation in the stomach often appears when hungry or before bedtime, making it difficult to sleep.

3. Laboratory diagnosis
3.1. Irritable Bowel Syndrome
- Blood test results are normal.
- Perform a fecal occult blood test or check for parasites.
- Abdominal ultrasound to detect abnormal tumors or signs of invasion, aiding differential diagnosis.
- CT or MRI of the abdomen are often used to identify physical lesions in the intestines.
- Colonoscopy to rule out other conditions such as polyps, diverticulosis, or colon cancer.
- Conduct a biopsy and histopathological examination.
3.2. Gastritis
- Perform blood, stool, or breath tests to detect H. pylori bacteria.
- Gastroscopy to capture images or signs of inflammation in the stomach lining.
- Gastrointestinal X-ray with contrast to check for lesions such as stomach ulcers.
4. Treatment of gastritis and Irritable Bowel Syndrome
4.1. Treatment of Irritable Bowel Syndrome
4.1.1. Non-pharmacological treatment
- Diet: Limit foods that can cause bloating, such as carbonated drinks, broccoli, cauliflower, cabbage, and fresh fruits.
- Additionally, patients should avoid gluten-containing foods like wheat, barley, and rye.
- Foods classified as FODMAPs (including fermentable sugars like lactose, fructans, and fructose) are not recommended for individuals with IBS.
- Therapies such as meditation, relaxation, and listening to music can help reduce stress and anxiety for patients.
- Exercise regularly and choose gentle workouts like yoga.
- Ensure to drink plenty of water, more than 2 liters per day.
- Maintain regular eating and living habits.
4.1.2. Pharmacological treatment
- Medications supporting the treatment of constipation include fiber supplements such as Natufib, along with Sorbitol, Lactulose, and Bisacodyl.
- For diarrhea: Patients can use Cholestyramine or Loperamide.
- Additionally, to reduce spasms, antispasmodic or anticholinergic medications like Dipropyline and Hyoscine butylbromide can be used.
- Treatment antibiotics, such as Rifaximin.
4.2. Treatment of gastritis
4.2.1. Non-pharmacological treatment
- Adopt a healthy and scientific diet. Avoid spicy, sour, excessively salty, or overly sweet foods. Avoid eating late at night (after 8 PM) and never skip breakfast.
- Maintain regular daily routines; ensure proper rest and sufficient sleep.
- Engage actively in regular exercise and physical activity.
- Reduce the use of non-steroidal anti-inflammatory drugs and antibiotics.
- Do not let yourself fall into a state of stress, anxiety or overthinking.
4.2.2. Pharmacological treatment
- Medications for gastric mucosal protection: Misoprostol, Rebamipide,...
- Antacids: Aluminum, Magnesium Hydroxide,...
- H2 Receptor Blockers: Famotidine, Ranitidine,...
- Proton Pump Inhibitors (PPIs): Omeprazole, Lansoprazole, Pantoprazole, Rabeprazole, Esomeprazole,...
- Smooth Muscle Spasm Relievers: Spasmaverine, Trimebutine,...
- H.Pylori treatment should follow guidelines.
Among the common digestive diseases nowadays, gastritis and irritable bowel syndrome (IBS) are two of the most prominent. Early detection and effective treatment can help patients and their families improve treatment outcomes and reduce the risk of serious complications.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.