This is an automatically translated article.
The article was consulted with Dr. To Kim Sang - Oncology Center, Vinmec Central Park International General Hospital.Meningiomas are the most common benign intracranial tumor. When the tumor grows large, it can cause neurological symptoms or threaten the patient's life. Therefore, patients need to be diagnosed with meningiomas early to receive timely and effective treatment.
1. What is a meningioma?
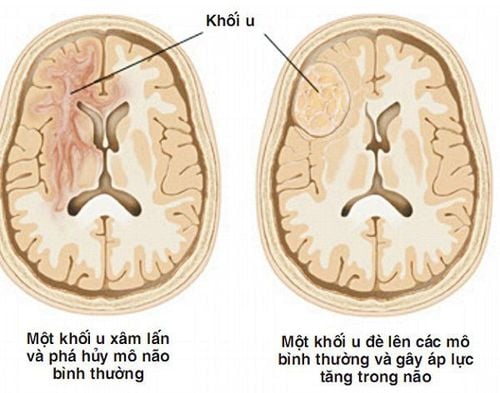
Meningioma is a primary tumor of the central nervous system that develops from the dura mater or arachnoid – the thin membrane that covers the brain and spinal cord. Meningiomas grow slowly, do not infiltrate (invasive) and push adjacent tissues. The majority of meningiomas are benign. However, they can grow to a very large size and in some special locations, can cause neurological symptoms (hemiplegia, visual disturbances, perceptual disturbances),... or threaten the patient's life.
Phần lớn các trường hợp mắc u màng não là lành tính
Cavernous sinus meningioma: Located near the area that drains venous blood from the brain to the heart; Hemispheric meningioma: Located on the surface of the cerebral hemisphere; Cerebellar pontine meningioma: Located near the cerebellar border; Intraorbital meningioma: Located in or around the orbit; Occipital meningioma: Located near the opening of the base of the skull, through which the lower part of the brain stem descends; Intraventricular meningioma: Located in the ventricles - where cerebrospinal fluid is drained to the entire brain; Olfactory sulcus meningioma: Located along the olfactory nerve; Meningiomas of the temporal bone: The temporal bone contains structures that support hearing; Meningiomas crescent brain / superior longitudinal sinus: Located next to the dural fold, the position separates the two hemispheres of the brain; Sphenoid meningioma: Located near the sphenoid bone, behind the eye socket; Spinal meningioma: Located in the spine, in some cases, it can compress the spinal cord; Posterior fossa meningioma: Located near the back of the brain; Pituitary meningioma: Located near the base of the skull, the pituitary gland is located; Meningiomas of the cerebellum tentacle: Located in the tent of the cerebellum.
2. Methods of diagnosing meningioma
2.1 Diagnosis based on clinical symptoms Depending on the location of the meningioma, the clinical presentation will be different. Manifestations of some types of meningiomas are:Meningiomas of the olfactory sulcus:
Having Foster Kennedy syndrome: Loss of smell, atrophy of the ipsilateral papillae and contralateral papilledema; Decreased vision; Urinary incontinence; Psychosis; Epilepsy. Crescent meningiomas, superior longitudinal venous sinuses:
Tumor in the anterior third of the body: Headache, mental disorders; Tumor in the middle third: Epilepsy, progressive paralysis of one limb; Tumor in the posterior third: Decreased vision, headache, partial seizures or psychosis.

Chẩn đoán u não dựa trên các triệu chứng lâm sàng
The tumor develops from the meninges along the sphenoid wing at the floor of the skull. Depending on the anatomical position, it can be distinguished into 2 types:
Tumor outside the sphenoid wing: Large-sized tumor easily causes headaches and seizures; Tumor inside the sphenoid wing: The tumor may enclose the optic nerve and the cavernous sinus, the internal carotid artery, and may damage the III, IV, V, and VI nerves. If the tumor spreads into the orbit, it can cause protrusion of the eyeball. Occipital meningioma:
Tumor progresses very slowly, often presenting as headache and damage to various cranial nerves.
Pituitary meningioma:
There are symptoms of visual acuity loss, bilateral hemiparesis, primary papilledema.
Meningiomas of the scapula:
The tumor develops on the supraclavicular surface, or is associated with the fossa Meckel and the ganglia of Gasser, causing the following symptoms:
Nerve pain V; If the tumor compresses the inferior temporal lobe, it can cause temporal epilepsy; If the tumor grows behind the scapula, nerves V, VII, and VIII may be damaged. Meningiomas on the stony slope:
May compress the pons, nerves and blood vessels at the stony slope; Manifestations of syndrome of increased intracranial pressure due to tumor compression of the circulation of cerebrospinal fluid. Symptoms include: headache, nausea, vomiting, double vision, increased blood pressure, shallow breathing, convulsions, confusion about time, loss of consciousness, coma. 2.2 Subclinical diagnosis of meningiomas Computerized tomography (CT scan) of the brain: Sometimes, doctors will use more contrast material during a CT scan to get a more accurate assessment. Manifestations of meningiomas on CT scan are co-dense, contrast-enhanced masses with extensive attachment to the dura. Calcified sand meningiomas may present on non-contrast film as 60–70 Hounsfield units, may have peritumoral cerebral edema or extend into the white matter of the whole hemisphere. Intraventricular meningiomas have 50% of cases with extraventricular edema.

Chụp CT để chẩn đoán lâm sàng u màng não
Manifestations of meningioma when taking MRI is where the tumor attaches to the dura with wide legs, a thin black line separating the tumor from the brain parenchyma and there is edema around the tumor. In addition, the diagnosis of meningiomas by MRI also helps determine the spread of the tumor directions, the relationship between the tumor and the adjacent neural structures, blood vessels and brain parenchyma.
Conventional skull X-ray: Manifestations of meningiomas on X-rays are:
Bone thickening or bone destruction; There are signs of dilatation of meningeal blood vessels; Calcified nodules of tumor. However, at present, with the development of modern imaging methods, conventional skull X-ray has low value in the diagnosis of meningiomas.
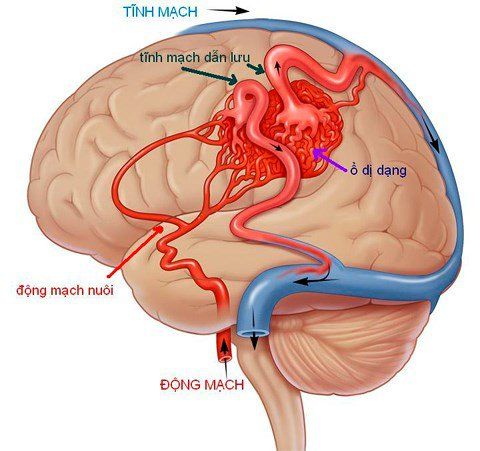
Angiography (cerebral angiogram): The characteristic of meningiomas is that the external carotid artery is the source of the tumor's blood supply, except for meningiomas in the olfactory sulcus and parapituitary meningioma that receive blood from the internal carotid artery. Suprapubic meningiomas are supplied with blood from the major branches of the ophthalmic artery. In addition, the meningeal artery branches of the anterior, middle, and posterior cerebral arteries are also the source of blood supply for meningiomas. Therefore, the method of cerebral angiography can be applied to diagnose meningioma.
Angiography is used to evaluate the condition of the veins or 4 large arteries that carry blood to the brain. During the test, the doctor inserts a long, flexible catheter into the blood vessels in the head and neck. Then, contrast dye is injected into the blood vessel through this catheter. Thanks to the contrast agent, the images of the arteries are clearly highlighted, showing details in the radiographs.

Phương pháp mạch não đồ để chẩn đoán u màng não
2.3 Anatomical diagnosis of meningiomas The anatomical classification of meningiomas is as follows:
Meningiomas: Including meningioma of the epithelium, transitional, fibrous, sandy, secretory forms, angiogenesis, microcapsule degeneration, clear cell, intact, metaplastic, lymphocyte-rich meningioma; Atypical meningiomas; Papillary meningioma; Malignant meningioma. 2.4 Differential diagnosis of meningiomas and other diseases Multifocal meningioma: A sign suggesting neurofibromatosis 2; Pleomorphic xanthoastrocytoma: Easily confused with meningiomas when the tumor is peripheral and may have a dural tail. When there are warning signs of meningiomas, patients should go to the hospital immediately to be examined, accurately diagnosed and have a timely and effective treatment plan, avoiding the risk of unpredictable complications. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.