This is an automatically translated article.
The article is written by MSc, BS. Mai Vien Phuong, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalEosinophilic esophagitis is not so common, so it is of little concern to patients, moreover the pathological symptoms are similar to many other common diseases, so the disease is often detected late, causing serious consequences for patients. patient health. Here are some early and effective methods of diagnosing the disease. Eosinophils are one of the components of white blood cells produced from the bone marrow and are one of the cells that play a role in promoting inflammation, especially allergic inflammatory reactions. Eosinophilic esophagitis (VTQDBCAT) is an eosinophilic infiltration of the esophagus that causes clinical symptoms.
1. Clinical symptoms
In children, common symptoms are similar to those of gastroesophageal reflux disease, including vomiting, abdominal pain, unwillingness to eat, slow weight gain... while in adults, three main symptoms are swallowing. difficulty swallowing, choking on food, and chest pain. Dysphagia may be present in 70-80% of patients while choking with food occurs in 33-54% of patients. This is followed by symptoms such as burning, reflux, heaviness in the chest, and chest pain when exercising. A review of 24 studies in Asian patients found that the most common symptom was dysphagia (55%), followed by burning (>20%). Other symptoms include epigastric pain, vomiting, chest pain, choking on food, reflux, abdominal pain, back pain.... When assessing disease activity, clinical symptoms cannot be relied upon alone. ready. A number of scales have been developed to assess disease activity in patients with VTQDBCAT such as EesAI index, PEESS questionnaire based on symptoms of dysphagia with different foods, but so far, people still The relationship between endoscopic severity and histopathology has not been demonstrated. The proportion of VTQDBCAT patients with other allergic diseases such as allergic rhinitis, asthma, eczema is higher than in the community. VTQDBCAT is considered a distinct form of food allergy due to reversible eosinophilic infiltrative esophagitis (BCAT) under strict dietary restrictions in which allergy mediated IgE is common with the rate of 15-43%.According to the natural progression of the disease, if left untreated, the symptoms will persist and the chronic inflammation will lead to the formation of fibrous rings or narrowing of the esophagus, thereby causing functional disorders. This affects the quality of life as well as the patient's social and psychological activities. To date, there is no evidence that VTQDBCAT is a risk factor for esophageal malignancy.
2. Subclinical
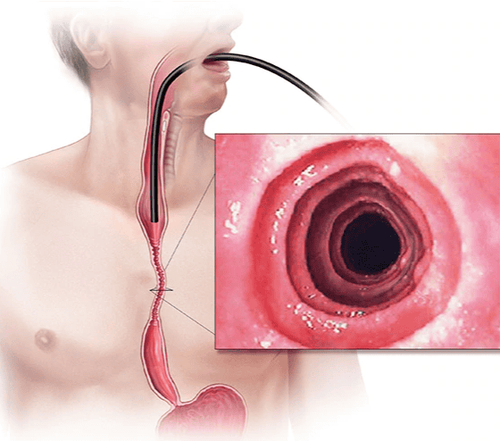
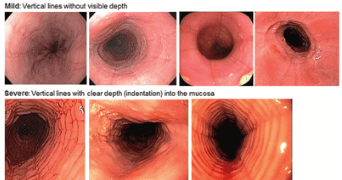
2.1. Upper GI endoscopy The endoscopic images of VTQDBCAT are quite diverse including white exudative plaques, concentric rings, narrowing, mucosal loss of capillary network, paper thin esophagus, Schatzki ring, pseudo-diverticulum and On endoscopic ultrasonography, thick esophageal wall can be seen. Endoscopy helps to assess disease activity by identifying inflammation (signs of edema, exudation, longitudinal groove of the esophagus) and narrowing (esophageal ring, stricture) and then decide on treatment. Interventional dilation of the esophagus when indicated as well as monitoring in response to treatment.However, the endoscopic method also has some limitations such as the sensitivity and specificity of the endoscopic images that vary based on the severity and number of lesions recorded, besides, there are 10 - 25% The patient had a normal endoscopic picture. In addition, most of the studies evaluating the benefit of endoscopy for VTQDBCAT did not exclude patients with GERD and those with PPI-responsive esophageal elevations of BCAT. Therefore, relying only on endoscopic images will not be able to diagnose VTQDBCAT as well as assess the extent of the disease.

2.3. Other imaging methods In recent years, there have been a number of studies applying computed tomography or endoscopic ultrasound in the evaluation of VTQDBCAT. On computed tomography, thickening of the esophageal wall can be seen. Some of the endoscopic ultrasound findings include loss of the usual layers of the esophageal wall or diffuse thickening of the esophageal wall due to inflammation and transluminal fibrosis or focal thickening of the muscularis or submucosa.
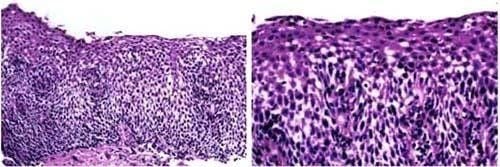
2.4. Histopathology Diagnosis of VTQDBCAT is generally based on esophageal biopsy results, with eosinophilic infiltration in the esophageal tissue. Biopsy through gastrointestinal endoscopy (inserting a small camera into the esophagus and then clicking on which point), usually performed by gastroenterologists. There are many other diseases that also cause eosinophilia in the esophageal tissue, including gastroesophageal reflux disease (GERD), parasitic infections, fungal infections, inflammatory bowel disease, cancer, and repeated episodes of vomiting. and some other diseases. Such conditions must be ruled out before EE is thought and diagnosed.
According to the definition of VQDBCAT released in 2011 and has been used uniformly up to now, this is a disease that is diagnosed not only based on histopathological results but also requires close coordination with clinical symptoms. and evaluate esophageal dysfunction.
3. Diagnosis
3.1. Determining diagnosis In the recommendations of the American Gastroenterology Association in 2011 and 2013, the diagnosis of VTQDBCAT requires a combination of clinical and pathological features (which cannot be separated by any criteria) including:Symptoms associated related to esophageal dysfunction. Inflammation with predominance of eosinophils in esophageal biopsies (215 eosinophils/1 field). Mucosal eosinophilic BC was localized only to the esophagus and persisted after a trial of PPIs (antacids). Exclude all causes of eosinophilia secondary to the esophagus. Response to treatments (modified diet, topical corticosteroids) is suggestive but not required in the diagnostic criteria. 3.2. Differential diagnosis The 2013 American Gastroenterology Recommendations highlighted that if eosinophilia is found in the esophagus, three possibilities should be raised: VTQTCAT, GERD, and esophageal eosinophilia that responds to antibiotics. PPI acid secretion (abbreviated as PPI-REE, is a pathology of unknown mechanism). Many studies have tried to find a way to differentiate between PPI-REE and VTQDBCAT. Both diseases have similar clinical, endoscopic and histopathological features. PPIs themselves also have anti-inflammatory effects, and some recent studies have shown that PPI treatment reduces Th2-mediated inflammation in PPI-REE patients similar to remission in VTQDBCAT patients. during topical steroid therapy. There are a number of features that can help differentiate GERD from VTQTBCAAT, but it should be noted that both GERD and VTQDBCAT are common in younger patients and can sometimes co-occur in the same patient. In patients with esophageal dysfunction for which the diagnosis of GERD has been established by endoscopy or pH measurement, VTQDBCAT cannot be completely ruled out. The relationship between GERD and VTQDBCAT is complex and can be bidirectional. It is hypothesized that when a patient has GERD, the permeability of the esophageal mucosa changes, making it more susceptible to the effects of allergens and triggering an immune response. In contrast, in patients with VTQDBCAT, there was increased sensitivity to the presence of acid on the esophageal mucosa compared with healthy subjects. Thus, VTQDBCAT can also induce structural and functional changes in the esophagus and cause secondary GERD.
Conclusion Pathology of VTQBCAT has not been diagnosed yet because the frequency of the disease is low, the symptoms sometimes overlap with other diseases in the esophagus, so it is easy to miss the disease. Patients with symptoms of difficulty swallowing, choking, chest pain... need to consult a specialist doctor for timely diagnosis and treatment.
To protect your health, you should check your general health regularly. Currently, Vinmec International General Hospital has general health checkup packages suitable for each age, gender and individual needs of customers with a reasonable price policy, including:
Health checkup package general Vip Standard general health checkup package Patient's examination results will be returned to your home. After receiving the results of the general health examination, if you detect diseases that require intensive examination and treatment, you can use services from other specialties at the Hospital with quality treatment and services. outstanding customer service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesLandres RT, Kuster GG, Strum WB (1978). Eosinophilic esophagitis in a patient with vigorous achalasia. Gastroenterology, 74(6): 1298 - 1301. 2. Lucendo AJ et al (2017). Guidelines on Esophageal eosinophiliaevidence based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J, 5(3): 335-58. 3. Straumann A, Spichtin HP, Bernoulli R et al (1994). Idiopathic eosinophilic esophagitis: a frequently overlooked disease with typical clinical aspects and endoscopic findings. Schweiz Med Wochenschr, 124: 1419 -29. Hirano I, Moy N et al (2013). Endoscopic assessment of the esophagus features of eosinophilic oesophagitis: validation of a novel classification and grading system. Gut, 62(4),: 489 -95