This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Manifestations of gastroesophageal reflux disease (GERD) have recently been classified as esophageal or extraesophageal syndrome. Clinical history, questionnaire data, and response to antisecretory therapy are not sufficient to make an accurate diagnosis of GERD. Endoscopy has low sensitivity. Recently, the advent of multichannel intraluminal impedance measurement and esophageal pH (MII-pH) monitoring have modified the diagnostic approach towards atypical manifestations of GERD. There is growing consensus that this technique should be considered the gold standard for diagnosing GERD.
1.About Gastroesophageal Reflux Gastroesophageal Reflux Disease (GERD) is one of the most common digestive disorders in Western countries. The clinical features of GERD have recently been classified as esophageal or extraesophageal syndrome. The most common atypical presentation of GERD may include ear, nose, and throat (ENT) symptoms, pulmonary (chronic cough or asthma) symptoms, or cardiac symptoms (noncardiac chest pain). Therefore, GERD should be strongly considered in the differential diagnosis of patients with atypical symptoms when alternative diagnoses have been ruled out by another specialist (ear, nose and throat surgeon, physician) cardiologist, pulmonologist, allergist).
The diagnosis of GERD is difficult and is usually made by a combination of clinical symptoms, response to acid suppression, as well as objective examination with upper gastrointestinal endoscopy and esophageal pH monitoring.
2. Role of esophageal manometry in difficult-to-diagnose GERD Esophageal manometry is now considered the gold standard test for diagnosing esophageal dysfunction that can cause symptoms such as difficulty swallowing and chest pain. However, it has shown limited ability to diagnose GERD. With the advent of high-resolution manometers, it is now possible to more accurately assess esophageal motility. Furthermore, new measures have been developed to investigate the morphology and function of the gastroesophageal junction (EGJ). In particular, the antireflux barrier function of the gastroesophageal junction can now be assessed by evaluating the contractility integral of the junction. In addition, transient lower esophageal sphincter dilation can be more accurately identified with high-resolution manometry. Neither lower esophageal sphincter pressure nor the presence of a motility abnormality are specific enough to diagnose GERD.
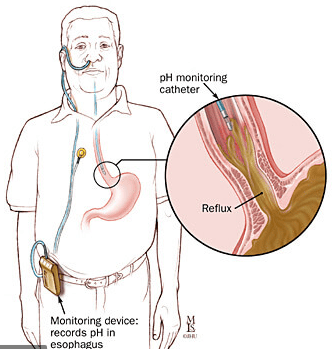
Role of 24-hour esophageal pH measurement in difficult-to-diagnose cases of GERD. Ambulatory reflux monitoring (24-hour esophageal pH measurement) is the only method that allows direct measurement of esophageal acid exposure (acid exposure time, acid exposure time), episode frequency regurgitation and the relationship between symptoms and episodes of reflux. It is commonly used to evaluate patients without endoscopic evidence of GERD, to confirm the diagnosis. It can also be used to monitor reflux control in people undergoing treatment with persistent symptoms.
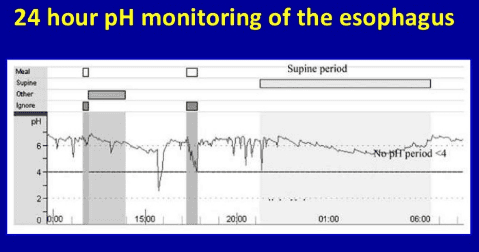
Principles of this method
24-hour esophageal pH measurement allows monitoring of the presence of acid in the esophagus to be recorded for 24 hours using a transnasal pH catheter placed near the lower esophagus. When there is movement of stomach acid into the esophagus during reflux, it lowers the pH of the esophagus. The test is considered positive if the pH drops below 4 for longer than 5 seconds. Patient tracing is analyzed and results are expressed using six standard components. Out of these 6 parameters, a pH score known as the DeMeester Score was calculated, which is a global measure of esophageal acid exposure.
Limitations of the method
There are limitations to the use of 24-h pH measurement for the diagnosis of GERD. The frequency of symptoms may vary. It is less likely that symptoms will occur during a routine 24-hour follow-up session and therefore a single measurement may not be representative. In addition, pH monitoring cannot diagnose non-acid reflux (pH > 4).
4. How is the data analyzed? 24-hour esophageal pH impedance monitoring is a technique used in the diagnosis of GERD, by monitoring both impedance and pH. An impedance pH probe is inserted into the nostril and into the esophagus. The impedance pH probe will stay in place for 24 hours and is connected to a small recorder.
Impedance measurement allows detection of upstream and countercurrent flow (liquid, gas or mixture) in the esophagus and combined pH monitoring allows chemical characterization of the refluxed substance. pH impedance monitoring can detect not only acidic (pH <4) but also weak acid (4
Upon completion of the impedance-pH study, the data are analyzed using appropriate software and the results are interpreted by the reporting physician. The software identifies individual reflux and swallow events, measures the association between symptoms and regurgitation, and distinguishes clinically unimportant impedance changes. Automated analysis is appropriate for acid reflux cases but overestimates non-acid or weak acid events. As a result, the Symptom Index (SI) and Symptom Association Probability (SAP) calculations may be affected. Manual review is recommended 2 minutes before each symptom event in pH impedance studies.
5. Acid exposure time (AET) – important factor in diagnosing atypical GERD Acid exposure time (AET) as a percentage of time pH less than 4 at esophageal pH sensor far. The Lyon consensus proposes that <4% acid exposure duration is considered completely normal (physiological) and >6% is considered completely abnormal. Intermediate values define a “gray area” in which additional evidence from other tests may provide for the presence of pathological acid burden. Furthermore, there is a significant daily variation in acid exposure time measurements so clinical decisions should never be made solely on this parameter.
Several authors have evaluated the correlation between the number of reflux episodes and GERD. Some episodes of markedly high reflux (above 80) may be considered abnormal while some episodes with a pH impedance of 40 or less are considered normal. However, the number of reflux episodes is not a predictor of treatment outcome but rather an aid.
6. Role of Acid Exposure Time (AET) in Clinical Diagnosis Symptom reporting during ambulatory 24-hour reflux monitoring allows investigation of the temporal relationship between reflux and symptoms . The pH impedance allows to modify the diagnostic analysis for atypical GERD manifestations such as cough, asthma, laryngitis, and noncardiac chest pain. Only symptoms that could reasonably be associated with reflux episodes such as cough, chest pain, heartburn, and regurgitation were considered to analyze the association between reflux symptoms. A reliable symptom association analysis cannot be performed for symptoms with no apparent onset and chronic presentation, such as dyspnea or hoarseness.
7. SI and SAP indices in 24-hour esophageal pH measurement The relationship between symptom events and reflux episodes can be assessed using SI and SAP. SI is defined as the percentage of symptomatic events related to reflux episodes, so the number of reflux-related symptomatic events divided by the total number of symptomatic events multiplied by 100%. The most commonly used cut-off level is 50%, which means that above 50% SI is considered positive. There is not necessarily a correlation between SI and acid exposure in the esophagus. The main defect of the SI is that it does not consider the total number of reflux episodes; therefore, the probability that the SI becomes positive increases as the number of reflux episodes increases. The SI introduces another limitation: it does not incorporate all the factors that determine the relationship between symptoms and reflux.
SAP is a statistical parameter that represents the relationship between symptom events and reflux episodes during measurement. The calculation is more complicated than the SI and cannot be done by hand, but it is calculated by measuring software instead. Limits for SAP of 95% and SAPs above 95% (corresponding to P < 0.05, applying Fisher's exact remainder on a 2x2 table) were considered positive for the relationship between prodromal events. symptoms and reflux episodes.
Limitations of the SAP index
These indices have some limitations, especially regarding the daily variation of reflux burden and the occurrence of symptoms during the follow-up day. The presence of positive SI and positive SAP together provides the best evidence of a clinically relevant association between reflux events and symptoms. If one test is positive and the other is negative, this represents a gray area and requires further interpretation with other clinical parameters and factors.
8. Classification of non-erosive GERD according to the 24-hour esophageal pH index Non-erosive reflux disease (NERD) represents the more common phenotypic manifestation of GERD and these patients are markedly heterogeneous in terms of pathophysiological score. By monitoring impedance-pH for 24 hours. This technique can identify three subtypes of NERD:
Patients with “true” NERD are characterized by duration of pathological acid exposure; Patients with esophageal hypersensitivity (HE) characterized by normal duration of acid exposure and positive acid SI/SAP or weak acid reflux; Patients with functional heartburn (FH) do not have any type of reflux underlying their symptoms and must be excluded from the scope of GERD.

According to Roma III, FH is not a GERD subcategory and it is classified as dysfunctional. Patients in groups 1 and 2 should be treated with a reflux inhibitor. Patients with functional heartburn should not be treated with PPIs.
Recent studies show the additional diagnostic value of two new pH impedance parameters, the refluxed peristaltic wave index (PSPW) and the mean nocturnal basal impedance (MNBI).
Chemical clearance includes salivation, which is stimulated by the postreflux esophageal vagal reflex and delivers salivary bicarbonate and epidermal growth factor to the esophagus, which raises the pH and rapidly Repair mucosal damage. peristaltic wave index due to regurgitation is defined as a 50% decrease in impedance occurring within 30 seconds of the reflux event, originating in the nearest impedance channel, reaching impedance positions furthest and followed by at least 50% back to baseline. An indicator of chemical clearance, specifically the reflux swallowing peristaltic wave index, was obtained by dividing the number of reflux swallowing peristaltic wave indices by the total number of reflux events.
The baseline impedance value reflects the permeability of the esophageal mucosa. Low basal esophageal mucosal impedance is associated with interstitial changes and tight junctions and reflux symptoms. The average nocturnal fundamental impedance is considered to be the furthest impedance channel during side-lying at night. Three 10-minute time periods (approximately 1 am, 2 am and 3 am) were selected, excluding swallow, reflux, and pH reduction; and the mean of the three measurements was calculated to obtain the average nocturnal fundamental impedance.
Reflux swallowing peristaltic wave index and nocturnal mean basal impedance
Reflux swallow peristaltic wave index and mean basal impedance at night increase the diagnostic yield of follow-up impedance-pH in GERD patients compared with healthy controls. The reflux swallowing peristaltic wave index had lower ERD values in NERD patients and in both groups compared with subjects without GERD. The mean nocturnal baseline impedance distinguishes PPI response to PPI refractory heartburn from common normal pH variables and is associated with a higher probability of PPI response in patients with chronic cough. In clinical practice, these novel impedance detection parameters can distinguish reflux-associated heartburn from nonreflux-related heartburn in patients of normal duration of acid exposure. The very high sensitivity of both parameters allows reflux disease to be ruled out when normal values are found.
Reflux swallowing peristaltic wave index and mean nocturnal basal impedance are also diagnostic in treating patients as assessed by impedance-pH monitoring. Reflux-induced peristaltic wave index and mean nocturnal baseline impedance effectively differentiate treatment-resistant PPI-NERD from FH.
Low mean nocturnal baseline impedance (<2292 Ω) independently predicts response to antireflux therapy. Frazzoni et al. hypothesized that the abnormal reflux-induced peristaltic wave index represents an independent predictor of treatment-resistant PPI-GERD, possibly because the defective esophagogastric-salivary tract was not affected. by surgical treatment. It is conceivable that a persistent decline in chemical clearance is clinically latent after successful surgery due to the subtotal elimination of reflux events, thus defining recovery. mucosal integrity, as indicated by improved mean nocturnal basal impedance and subsequent remission of persistent heartburn.
If you need to consult and visit at hospitals and clinics of Vinmec Health system nationwide, please contact the Website for the best service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesCesario Silvia,1 Scida Serena, et al., Diagnosis of GERD in typical and atypical expressions, Acta Biomed. 2018; 89(Suppl 8): 33–39. El-Serag Hashem B, et al. “Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review” Gut. 2013 gutjnl-2012. [PMC free article] [PubMed] [Google Scholar]