This is an automatically translated article.
Coma due to ketoacidosis in diabetic patients is a dangerous complication, which can seriously affect the patient's life. The main cause of this condition is lack of insulin, which causes severe disturbances in protein, lipid and carbohydrate metabolism.
1. What is diabetic ketoacidosis?
Ketogenic coma is a medical emergency, a serious complication of severe insulin deficiency in patients with diabetes mellitus. The pathogenic mechanism includes three dangerous metabolic disorders including: hyperglycemia, acidosis due to the presence of ketones in the blood and electrolyte disturbances.
1.1 Increased blood sugar
Due to insulin deficiency combined with increased production of insulin antagonist hormones, neoglucose in the blood, reducing glucose utilization in peripheral tissues, consequent elevation of blood glucose levels.
1.2 Ketoacidosis
The lack of insulin and the increase in insulin antagonist hormones (glucagon, catecholamines, cortisol) increase the lysis of adipose tissue, release of free fatty acids and the formation of ketone acid bodies (acetone, acetoacetic acid and acid 3). -beta-hydroxybutyric). As a result, the alkaline reserve in the body is reduced, and the blood acidosis is severe.

Nhiễm toan ceton gây hôn mê nhiễm toan ceton ở bệnh nhân đái tháo đường
1.3 Disorders of water and electrolytes
Patients with diabetes leading to ketoacidosis will cause osmotic polyuria due to increased sugar in the urine and severe dehydration of the body and electrolytes.
2. Predisposing factors for ketoacidosis
Many patients with diabetes develop ketoacidosis without a known trigger.
Patients with type 1 diabetes who are on insulin therapy but suddenly stop insulin, or who are taking insulin but have a number of additional predisposing factors leading to complications of ketoacidosis coma. Patients with type 2 diabetes have poorly controlled blood glucose levels with predisposing factors to ketoacidosis. Predisposing factors include:
Infections in the body such as pneumonia, meningitis, intestinal infections, urinary tract infections... Trauma Stroke Heart attack Stroke Cerebrovascular accident Use of drugs there's cocaine...
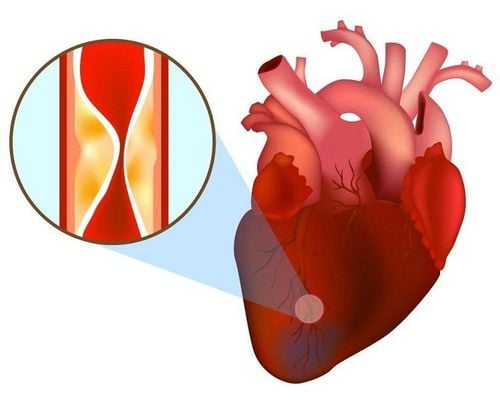
Bệnh nhân nhồi máu cơ tim tăng nguy cơ nhiễm toan ceton
3. Diagnosing ketoacidosis in diabetic patients
3.1 Clinical signs and symptoms of the disease
Patients often feel nauseous and vomit a lot. Feeling thirsty, drinking water, and urinating more often than usual. Feeling tired, loss of appetite. Change vital signs such as tachycardia, hypotension, shallow tachypnea with Kussmaul breathing. Signs of dehydration, hot dry skin. Confusion or impairment of consciousness such as drowsiness, lethargy or coma A very specific sign is the smell of ketones in the patient's breath.
3.2 Subclinical signs
Blood glucose > 13.9 mmol/L. Bicarbonate (plasma) <15 mEq/L. Arterial blood pH < 7.2 Presence of acid ketone bodies in blood and urine.
Glucose máu > 13.9 mmol/L là dấu hiệu của nhiễm toan ceton trên bệnh nhân đái tháo đường
4. Treatment of ketoacidosis in patients with diabetes
4.1 Compensation for water loss
The presence of glucose in the urine causes osmotic polyuria, leading to dehydration and electrolyte loss in all diabetic patients with ketoacidosis. Rehydration is very important, the rehydration regimen is as follows:
1st hour: 0.9% NaCl solution: 15-20 mL/kg (500 mL/m2 skin/hour). If the patient is elderly or has heart disease, this volume may be lower. 2nd hour: 0.9% NaCl solution 15 mL/kg. In case the patient has hypernatremia or congestive heart failure, use 0.45% NaCl hypotonic solution. 3rd hour: Reduce fluid intake to 7.5 mL/kg/hour (adults) or to 2-2.5 mL/kg/hour (infants). The type of solution used in this stage is usually a hypotonic solution of 0.45% NaCl. Hour 4: Depending on the clinical development, consider the amount of fluid in and out. When the patient's blood glucose is about 13.9 mmol/L (250 mg/dL), 0.9% NaCl can be replaced with a 5% glucose solution while insulin is continued, or an isotonic saline solution is used. stretch. Rehydration is continued until the patient's condition improves, vomiting is reduced, and oral feeding is possible.
4.2 Use of insulin
The main mechanism of ketoacidosis in diabetic patients is still severe insulin deficiency. Therefore, insulin compensation is a necessary and important factor in the treatment of diabetic ketoacidosis.
The type of insulin used in an emergency is a rapid-acting insulin (also known as regular insulin) and administered intravenously (injection or infusion). The therapeutic dose with insulin is as follows:
Initial dose is 0.1-0.15 IU/kg/hour (intravenous) Then continue intravenous infusion at a dose and rate of 0.1 IU/kg/hour. Some notes when it is necessary to change the dose and rate of insulin infusion: If the patient has no response after 2-4 hours of using insulin, the blood glucose cannot decrease by 3.9 mmol/L/hour, the infusion dose must be doubled. . If blood glucose is < 13.9 mmol/L (250 mg/dL), the insulin infusion dose should be reduced, adding 5% glucose solution (Dextrose 5%).

Sử dụng insulin giúp điều trị nhiễm toan ceton ở bệnh nhân đái tháo đường.
Conditions for switching from intravenous insulin to subcutaneous insulin when the patient is awake and able to eat by mouth:
Clinical signs improve. Blood pH > 7.3, plasma bicarbonate concentration > 18 mEq/L, electrolytes returned to normal. Patients can eat and drink, no longer vomiting or nausea. Predisposing factors for disease onset (such as infection, trauma, etc.) have been well controlled. When switching to subcutaneous injection, a medium-acting insulin should be used and the dose of insulin depends on the blood glucose level.
4.3 Potassium compensation
A common electrolyte disturbance in patients with ketoacidosis is hypokalemia (incidence 50%). It is caused by renal loss of potassium (due to osmotic polyuria, loss of reabsorption) or by vomiting, diarrhea... Consider the following factors before performing potassium replacement:
Illness Does the patient have kidney failure? If in the first hour, the patient can urinate ≥ 60ml/hour, the kidney function is still good. What is the current blood potassium level? Electrocardiogram monitoring. Indications for potassium replacement:
Blood potassium > 5.5 mmol/L: No potassium infusion Blood potassium from 3.5 to 5.5 mmol/L: compensate 20 mmol K+/liter of infusion Fluid Serum potassium < 3.5 mmol/L: compensate 40 mmol K+/liter IV fluids Absolutely do not use intravenous insulin if the blood potassium level is less than 3.3 mmol/L.
5. Notes in the treatment of ketoacidosis in patients with diabetes
It is necessary to find and treat the factors that favor the onset of ketoacidosis in patients with diabetes such as trauma, stress, infection... The patient needs comprehensive care, especially when the patient is comatose. Prevention of common complications during treatment. Recurrent ketoacidosis has a much worse prognosis. Cerebral edema and even death can occur. To be on the safe side, a blood glucose level should be maintained around 11.1 mmol/L (200 mg/dL) for the first 12-24 hours. Vomiting and nausea cause aspiration of food, which can lead to aspiration pneumonia. Hypoglycemia may occur. As a precaution, blood glucose should be maintained at 11.1 mmol/L - 13.9 mmol/L. Fluid replacements (especially isotonic salts) may increase congestive heart failure.

Bệnh nhân nhiễm toan Ceton trong tình trạng hôn mê cần được chăm sóc đặc biệt
6. Prevention of ketoacidosis in patients with diabetes
Patients should be taught how to self-monitor blood glucose levels. Go to the doctor right away when the body shows abnormal signs such as nausea, fever, abdominal pain, diarrhea or high blood glucose levels... or there is another medical condition such as infection, injury, pregnancy. ... Adhere to treatment, do not arbitrarily reduce insulin dose, or arbitrarily quit even when suffering from another disease. Currently, Vinmec International General Hospital is providing a diabetes screening package to help patients detect the disease early and improve treatment efficiency.
To register for an examination at Vinmec International General Hospital, you can contact the nationwide Vinmec Health System Hotline, or register online HERE.













