This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Endoscopy is the main method for early gastric cancer screening because of its high detection rate, however, the diagnostic accuracy is highly dependent on the availability of endoscopic instruments. Many new endoscopic techniques have been shown to increase the likelihood of early gastric cancer diagnosis.
With improved early gastric cancer detection rates, endoscopic treatment has gained popularity due to advances in existing equipment and the experience of endoscopists. The purpose of this review is to summarize the endoscopic diagnosis and treatment commonly used in early gastric cancer (early gastric cancer).
1. Introduction to early gastric cancer
Stomach cancer is the fourth most common cancer worldwide and the second leading cause of cancer death. With increasing public awareness of early cancer diagnosis and treatment as well as the development of endoscopic imaging and imaging enhancement techniques, such as magnified narrowband imaging, endoscopic staining color and confocal laser endoscopy, the rate of early gastric cancer at diagnosis is increasing. Early detection is essential for treatment. It has been shown that the prognosis of early gastric cancer is excellent with 5-year survival rates above 90%.
Trắc nghiệm: Bạn có biết những sự thật này về dạ dày không?
Hoạt động của dạ dày là một hoạt động quan trọng giúp cơ thể dung nạp và chuyển hóa dinh dưỡng từ thực phẩm hàng ngày. Tuy nhiên, không phải ai cũng biết rõ về dạ dày cũng như các vấn đề xoay quanh hoạt động tiêu hóa thức ăn của nó. Hãy cùng tìm hiểu kỹ hơn trong bài trắc nghiệm dưới đây.
Bài dịch từ: webmd.com
2. PARIS classification of superficial cancerous lesions in the gastrointestinal tract
According to the PARIS classification of superficial cancerous lesions in the gastrointestinal tract, type 0 is divided into three categories corresponding to convex lesions (0-I), non-convex and non-concave lesions (0-II), and concave lesions (0-III). Type 0-I is divided into pedunculated (0-Ip) and sessile (0-Is) lesions. Type 0-II is divided into three subtypes, a, b, and c, corresponding to slightly elevated, flat, and concave lesions. Type 0-III are all ulcers. Mixed patterns with elevation and concavity also occur and are classified into two groups: in 0-IIc + 0-IIc lesions, most of the surface is concave; elevation present in a segment of the lesion in the periphery; in 0-IIa + 0-IIc lesions, there is a central depression in a globally elevated lesion. The combined excavated and indented patterns are referred to as 0-III + IIc or 0-IIc + III, depending on the respective surface of the ulcer and of the indented area.

The highest risk of invasion is seen in convex (0-I) or concave (0-IIc) lesions. The association between depth of invasion into the submucosa and lymph node metastasis was analyzed in 1091 cases at the National Cancer Center Hospital in Tokyo. When the invasion to the underlying layer was less than the cut-off limit of 500 μm, the rate was only 6%; beyond this limit it increases to 21% .
Endoscopic techniques for early gastric cancer treatment include endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). Outcomes of endoscopic mucosal resection in early gastric cancer are comparable to those of surgery in selected cases. Endoscopic submucosal dissection has been shown to increase the likelihood of total resection regardless of their size, location, or presence of scarring. As a type of minimally invasive endoscopic technique, endoscopic submucosal dissection is characterized by less trauma and complications and better treatment efficacy.
3. The role of diagnostic endoscopy
The Chinese guideline “Chinese consensus on diagnosis, treatment and endoscopic screening for early gastric cancer 2014” recommends high-risk populations: (1)> 40 years old; (2) Helicobacter pylori infection; (3) previous precancerous diseases such as chronic atrophic gastritis, gastric polyps, peptic ulcer, pernicious anemia; and (4) other high risk factors such as alcohol, smoking, high salt, preserved foods.
White light endoscopy (conventional white light endoscopy) can only detect obvious morphological changes of cancerous lesions, such as changes in their color (red), surface contour , or the kinetic response to gas injection/suction. Early gastric cancer can be divided into 3 types: superficially raised and concave. Shallow type is subdivided into raised appearance, flat appearance and concave appearance. Superficial flat lesions are difficult to find during routine white light endoscopy, often causing misdiagnosis and missed diagnoses. The most common lesions of early gastric cancer usually present with congestion and ulceration.
Endoscopic ultrasound (EUS) is used to examine the exact structure of each layer of the stomach wall. It can be used to assess the depth of invasion of early gastric cancer or to assess lymph node metastasis, providing evidence for treatment options. Fluoroscopy can identify precancerous and some hidden lesions on the basis of fluorescence. However, the high demand for the device leads to higher testing costs, making routine clinical use impossible or limited.
This review aims to summarize the endoscopic diagnostic and therapeutic methods commonly used in early gastric cancer, such as magnified endoscopy with narrow band imaging (Enlarged endoscopy with imaging). narrow band ), confocal laser endoscopy (Confocal laser endoscopy), endoscopic mucosal resection and endoscopic submucosal dissection.
3.1. Magnified endoscopy with narrow band imaging Magnified endoscopy with narrow band imaging (Enlarged endoscopy with narrowband imaging) is a recently developed technique that combines magnified endoscopy and imaging. narrow band image. It is widely used in early gastric cancer detection based on the basic microbiological findings of the microvascular structure (microvascular) and microstructure (microsurface) of the superficial mucosa. outside. The gastric mucosa is composed of glandular epithelium, which is different from normal glands. There are different classification systems to describe the correlation between microscopic images and actual images displayed by magnified endoscopy with narrowband imaging.
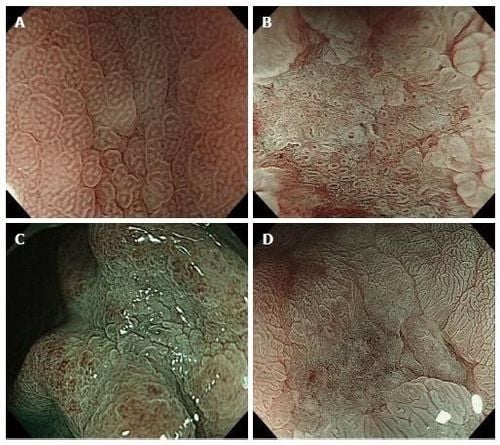
Kobara et al. and Kikuchi et al. report that magnified endoscopy with narrow band imaging can be used to determine the depth of invasion in gastric cancer. Kobara et al described three indices: unstructured, distributed and multidimensional ships. They suggest that the presence of all three indicators or the presence of two or more with magnified endoscopy with narrow band imaging should be considered as diagnostic criteria of the submucosal layer (SM2) for concave gastric cancer. Kikuchi et al found that the presence of dilated vessels (vessels 3 times the diameter of the irregular microvessels commonly observed in lesions) should be used to predict cancer. submucosal carcinoma; The specificity and negative predictive value (NPV) are close to 90%, but the sensitivity of vasodilatation is only 37.5%. Kiyotoki et al compared Magnified Endoscopy with narrowband imaging and indigo-stained endoscopy (ICC) to evaluate tumor margins and found that the correct ratio produces Magnified Endoscopy with high narrowband imaging. significantly more than ICC (97.4% vs 77.8%; P = 0.009).
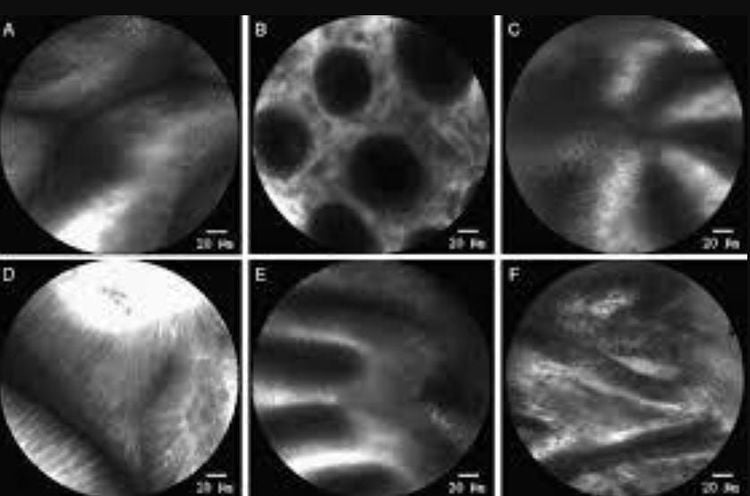
3.2 The role of confocal laser magnifying endoscopy in early gastric cancer diagnosis Confocal laser magnifying endoscopy (CLE) is a newly developed endoscopic imaging technology that produces facial images 1000x magnification cross section of GI surface and subsurface tissue. It is capable of providing direct histological observation of tissue in vivo without biopsy and distinguishing malignant from benign lesions in real time at the cellular level.

Gastric fossa is the smallest unit of the gastric mucosal surface and the smallest structural unit in confocal images. It presents as different images in different disease states.
According to the classification of gastric pit models by Zhang et al., gastric pit models are divided into 7 categories. Normal mucosa with basal glands mainly contains round pits (type A). Type G is commonly found in gastric cancer under confocal laser endoscopic imaging, with a sensitivity and specificity for gastric cancer of 90% and 99.4%, respectively. Type G1 is defined as loss of normal gastric pits accompanied by the presence of diffuse atypical cells, such as sigmoid ring cell carcinoma and low-differentiated ductal adenocarcinoma. Type G2 is represented by loss of normal pits with the appearance of atypical glands, mainly in well-differentiated ductal adenocarcinoma. Confocal laser endoscopy has great advantages in microvascular imaging, as the blood vessels of normal and cancerous mucosa have different characteristics under Confocal Laser Endoscopy. Currently, the cellular and tissue structural and vascular changes of confocal laser endoscopy in the diagnosis of gastric mucosal lesions are based on sodium fluorescence staining.
A prospective study including 1786 patients was performed by Li et al to evaluate the efficacy and reliability of confocal laser endoscopy in the identification of gastric surface cancerous lesions. They found that confocal laser endoscopic diagnosis for early gastric cancer had high sensitivity (88.1%) and specificity (98.6%).
Kakeji et al examined normal and 27 gastric cancer tissues ex vivo. Compared with histological results, confocal laser endoscopy has high diagnostic accuracy of 96.4%, sensitivity and specificity of 92.6% and 100%, respectively. Kitabatake et al. obtained in vivo confocal laser endoscopic images from normal mucosa and cancerous lesions in 27 patients with early gastric cancer and demonstrated sensitivity 81.8%, specificity 97.6%, and 94.2% accuracy.

Vinmec International General Hospital is equipped with the most modern flexible endoscopic system of Olympus - Japan. Narrow Banding Imaging (NBI) has made a breakthrough in the screening and diagnosis of cancers of the gastrointestinal tract (esophagus, stomach, duodenum, colon, rectum). in the early and very early stages. NBI endoscopic images have high resolution and contrast, so it is easy to detect small changes in color, morphology of cancerous and precancerous lesions that are difficult to detect with conventional endoscopy.
Standard treatment techniques, ensuring safety and quality of treatment for patients. The combination of a team of qualified and experienced specialists with a modern diagnostic endoscopy system, including the NBI narrow-band endoscopy system, you will enjoy the complete quality of service. Good quality and good diagnostic and treatment quality for gastrointestinal tract diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Jemal A., Bray F., Center M. M., Ferlay J., Ward E., Forman D. Global cancer statistics. CA Cancer Journal for Clinicians . 2011;61(2):69–90. doi: 10.3322/caac.20107. [PubMed] [CrossRef] [Google Scholar] Min Y. W., Min B.-H., Lee J. H., Kim J. J. Endoscopic treatment for early gastric cancer. World Journal of Gastroenterology. 2014;20(16):4566–4573. doi: 10.3748/wjg.v20.i16.4566. [PMC free article] [PubMed] [CrossRef] [Google Scholar] Oliveira F. J., Furtado H., Furtado E., Batista H., Conceicao L. Early gastric cancer: report of 58 cases. Gastric Cancer . 1998;1(1):51–56. doi: 10.1007/s101200050054. [PubMed] [CrossRef] [Google Scholar] Ono H., Kondo H., Gotoda T., et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut . 2001;48(2):225–229. doi: 10.1136/gut.48.2.225. [PMC free article] [PubMed] [CrossRef] [Google Scholar] Linlin Zhu, 1 Jinyu Qin,, Early Gastric Cancer: Current Advances of Endoscopic Diagnosis and Treatment, Gastroenterol Res Pract. 2016; 2016: 9638041.