This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalWith improved early gastric cancer detection rates, endoscopic treatment has gained popularity due to advances in existing equipment and the experience of endoscopists. The purpose of this review is to summarize the endoscopic diagnosis and treatment commonly used in early gastric cancer (early gastric cancer).
1. Endoscopic treatment of early gastric cancer lesions
New NCCN guidelines recommend that endoscopic mucosal resection or endoscopic submucosal dissection of early gastric cancer may be considered appropriate therapy when lesions are present. diameter ≤2 cm; It is shown histopathologically that it is well or moderately differentiated, does not penetrate beyond the superficial submucosa, exhibits no lymphatic invasion, and has clearly lateral and deep margins. But the guidelines do not specify when endoscopic mucosal resection is indicated and when endoscopic submucosal dissection is indicated.2. Signs of cancerous lesions that cannot be removed through endoscopy
The following are risk factors in case of endoscopic treatment, which may not be endoscopically resectable, lesions that cannot be raised after submucosal saline injection (non-elevation sign), Early gastric cancer with lymph node metastasis, cancer invading the muscularis stroma, and severe coagulation dysfunction. Age is not a risk factor, except in cases of severe organ failure. Anticoagulation should be discontinued 5–7 days prior to the procedure.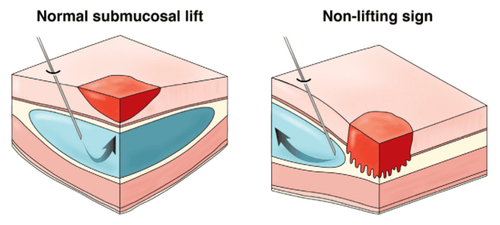
3. Endoscopic mucosal resection
Endoscopic mucosal resection was first applied to endoscopic therapy in 1984 by means of a strip biopsy (two-channel method). The procedure involves submucosal injection below the lesion, excision, and excision of the lesion. This lifting injection method is very simple and convenient. However, it is difficult to trap flat lesions. Furthermore, metal noses are prone to slippage, which can lead to incomplete excision and local recurrence. Endoscopic mucosal resection after circumcision was described by Hirao et al. in 1988.EMR technique – endoscopic mucosal resection Endoscopic mucosal resection with cap X-ray was developed in 1992. This technique can safely remove intramural cancerous masses 2cm or less in diameter using a clear plastic cap that is connected to the end of the endoscope. The procedure involves submucosal injection, aspiration of the lesion to the flap, capture, and excision. The operating procedure of endoscopic mucosal resection with ligation (EMR -L) is similar to that of endoscopic mucosal resection with a cap. The device for ligation endoscopic mucosal resection is the standard ligation device. After suctioning the lesion to the flap, an elastic band was deployed underneath the lesion, and then the banded lesion was tied and removed. Traditional endoscopic mucosal resection procedures (mentioned above) cannot remove flat lesions larger than 2cm at a time. This type of lesion can be removed by endoscopic partial mucosal resection (EPMR). However, it is difficult to graft resected samples in vitro and evaluate the effect of radical resection after EPMR.

4. Recommendations of the Society of Gastrointestinal Endoscopy of Japan
The Japan Gastrointestinal Endoscopy Society (JGES) in collaboration with the Japan Gastric Cancer Society (JGCA) have created guidelines for endoscopic submucosal dissection and mucosal resection. endoscopically for early gastric cancer treatment in 2015. The protocol recommends that endoscopic resection should be performed when the likelihood of lymph node metastasis is very low and the lesion size and site are both subject to resection. Monolithic . Endoscopic therapy (endoscopic mucosal resection or endoscopic submucosal dissection) is absolutely indicated in differentiated macromucosa (cT1a) carcinomas less than 2 cm in diameter. The macroscopic type is not important, but no ulcer (scar) was found, ie, UL (-).5. Efficacy of monolithic resection in early cancer treatment
The results of endoscopic mucosal resection showed 56%-75.8% monolithic and 66.1%-77.6% total excision abroad. A Japanese multicenter study of endoscopic mucosal resection in early gastric cancer showed that the rate of complete resection was related to lesion size; The rate of complete resection of lesions less than 1 cm was 82.4%, while only 16.2% of lesions larger than 2 cm were completely resected. Another Japanese document reported that both the 5-year and 10-year survival rates of patients with early gastric mucosal cancer less than 2 cm were completely removed by transendoscopic mucosal resection. soi is 99%. The risk of local recurrence after endoscopic mucosal resection ranges from 2% to 35% in Japan. Horiki et al found that the local recurrence rate of early gastric cancer after partial endoscopic mucosal resection was 30% (95% CI, 20–40%) at both 5 and 10 years. . Additional surgery is performed immediately after the initial endoscopic mucosal resection if the resection rate is clearly positive for cancer. Furthermore, determining the margin of resection is a problem in partial mucosectomy.6. Indications for submucosal dissection endoscopic technique
For the indications for endoscopic submucosal dissection, according to the recent Japanese Stomach Cancer guidelines 2015 and ESMO-ESSO-ESTRO 2013, in addition to the indications for mucosal resection, endoscopically, the indications for endoscopic submucosal dissection include the following:UL(-)cT1a with differentiated carcinoma greater than 2 cm in diameter. UL(+)cT1a differentiated carcinoma less than 3 cm in diameter. UL(-)cT1a undifferentiated carcinoma less than 2 cm in diameter. The extremely low risk of lymph node metastasis and the potential for expansion in the absence of lymphatic infiltrates (ly, v) together with the above criteria are very reasonable. Possibility of subsequent treatment of locally recurrent mucinous carcinoma under extended indication (level of evidence V, recommendation C1) if a lesion is within the indication for transmucosal submucosal dissection. endoscopic or primary endoscopic mucosal resection.
7. Efficacy of endoscopic submucosal dissection and endoscopic mucosal resection
According to the literature, the tumor resection rate of endoscopic submucosal dissection for early gastric cancer is 94.9%–97.7% and the 5-year survival rate is 83.1. % –97.1%. A multicenter retrospective study comparing laparoscopic mucosal resection and endoscopic submucosal dissection with resection in early gastric cancer reported that a single resection rate was significantly higher with endoscopic submucosal dissection than with endoscopic mucosal resection (92.7% vs 56%).Perforation rates were 3.6% with endoscopic submucosal dissection and 1.2% with endoscopic mucosal resection, although complications were managed endoscopically.
The 3-year cumulative residual/no recurrence rate of endoscopic submucosal dissection is 97.6%. In another study by Toyonaga et al involving 1136 patients with gastric cancer, the resection rate was 97.1%, the bleeding and perforation rate was 3.6% and 1.8%, respectively. , and the 3-year and 5-year survival rates were 91.7% and 88.1% respectively.

8. Complications of technique
Major postoperative complications of endoscopic submucosal dissection include bleeding, perforation, and stricture. The rate of acute intraoperative bleeding is 3.1-15.6% and the rate of slow bleeding is 3.1%~15.6%.Bleeding may be related to lesion size greater than 4 cm or thick submucosal blood vessels located in the upper 2/3 of the stomach. Perforation rate of endoscopic submucosal dissection is 1.2%–4.1%; The risk factor for perforation is lesions larger than 2 cm.
According to a study performed by Coda et al., the rate of restenosis after endoscopic submucosal dissection procedure was 17% (7/41), while pyloric stenosis was 7% ( 8/115) occurred after endoscopic submucosal dissection. The study identified the following as risk factors for stenosis, surface defect mucosal circumference reaching more than 3/4, or mucosal resection length more than 5 cm.
Vinmec International General Hospital is equipped with the most modern flexible endoscopic system of Olympus - Japan. Narrow Banding Imaging (NBI) has made a breakthrough in the screening and diagnosis of cancers of the gastrointestinal tract (esophagus, stomach, duodenum, colon, rectum). in the early and very early stages. NBI endoscopic images have high resolution and contrast, so it is easy to detect small changes in color, morphology of cancerous and precancerous lesions that are difficult to detect with conventional endoscopy.
Standard treatment techniques, ensuring safety and quality of treatment for patients. The combination of a team of skilled and experienced specialists with a modern diagnostic endoscopy system, including the NBI narrow-band endoscopy system, you will enjoy the perfect service quality. Good quality and good diagnostic and treatment quality for gastrointestinal tract diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References1. Jemal A., Bray F., Center M. M., Ferlay J., Ward E., Forman D. Global cancer statistics. CA Cancer Journal for Clinicians . 2011;61(2):69–90. doi: 10.3322/caac.20107. [PubMed] [CrossRef] [Google Scholar]
2. Min Y. W., Min B.-H., Lee J. H., Kim J. J. Endoscopic treatment for early gastric cancer. World Journal of Gastroenterology. 2014;20(16):4566–4573. doi: 10.3748/wjg.v20.i16.4566. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Oliveira F. J., Furtado H., Furtado E., Batista H., Conceicao L. Early gastric cancer: report of 58 cases. Gastric Cancer . 1998;1(1):51–56. doi: 10.1007/s101200050054. [PubMed] [CrossRef] [Google Scholar]
4. Ono H., Kondo H., Gotoda T., et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut . 2001;48(2):225–229. doi: 10.1136/gut.48.2.225. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Linlin Zhu, 1 Jinyu Qin,, Early Gastric Cancer: Current Advances of Endoscopic Diagnosis and Treatment, Gastroenterol Res Pract. 2016; 2016: 9638041.