This is an automatically translated article.
This article was written by Specialist Doctor II Khong Tien Dat, Doctor of Radiology - Department of Diagnostic Imaging - Vinmec Ha Long International Hospital.CT scan to diagnose cranial bone lesions with dural hematoma is the first thing to do when receiving patients with traumatic brain injury. The signs on the CT film will allow the neurosurgeon to guide the patient's surgical intervention, limiting the sequelae of brain damage.
1. What is an epidural hematoma?
An epidural hematoma is when blood forms between the inner surface of the skull and the outer layer of the dura. This condition is often associated with a history of head trauma and skull fractures. Circumstances where injuries occur are in traffic accidents, occupational accidents and also in daily life with falls, playing strong and antagonistic sports. The source of bleeding is usually from the artery, the most common is the ruptured middle meningeal artery due to trauma, accounting for 75%. Occasionally, a dural hematoma can originate from venous blood, when a ruptured venous sinus is the result of a fracture of the skull or maxillofacial region.A large or progressive dural hematoma can cause increased intracranial pressure, damage to the brain parenchyma, and most severely, mass brain herniation. In this situation, the central nervous functions of the patient will gradually decline, including consciousness. If the vasomotor and respiratory centers are also inhibited, the patient's life will become critical. Therefore, when a patient has a history of head trauma, an epidural hematoma needs to be quickly diagnosed and intervened as soon as possible.
2. What are the symptoms of a dural hematoma?
Anytime it is found that a person has had a head injury leading to a brief loss of consciousness or if there are any other symptoms after the head injury without loss of consciousness, the patient should be admitted to the hospital immediately to confirm the presence of a concussion. dural blood or not. The early intervention of epidural hematoma will have prognostic significance for the patient in the long term.If there is no loss of consciousness, the most important symptoms of a dural hematoma that should also be monitored are:
Headache Dizziness Irritability, restlessness Nausea, vomiting Drowsiness, somnolence Pussy dilated one eye Weakness of the limbs Transient loss of consciousness followed by awakening but quickly becoming unconscious The above symptoms usually occur within minutes to hours of the head injury. However, in the elderly, manifestations appear later, possibly up to days or weeks, and it is easy to miss this diagnosis when the history of head trauma is forgotten.
Chóng mặt là triệu chứng phổ biến của tụ máu màng cứng
3. How does a CT scan diagnose dural hematoma?
In adults, an epidural hematoma can form when an injury tears the arteries or veins that run along the inner wall of the skull. Sometimes injury to these blood vessels is accompanied by a skull fracture. Bleeding cases secondary to arterial trauma leading to an epidural hematoma will be larger in size and grow faster than an epidural hematoma that occurs after venous injury.Epidural hematoma in children is somewhat different from that in adults. The middle meningeal artery is not as firmly attached to the bone as in adults, so it is easy for epidural hematomas to occur from the edges of a fracture, and they sometimes occur at the same time in different locations.
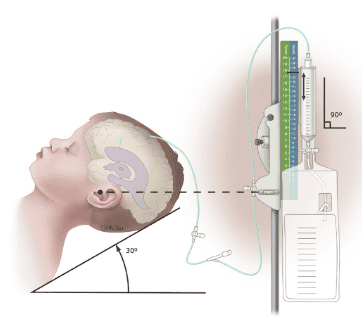
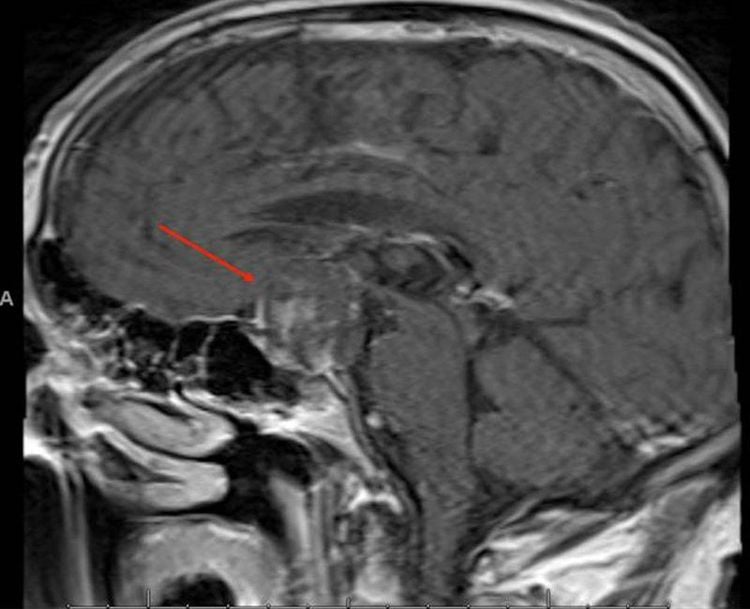
However, regardless of the subject, a CT scan of the brain is always the first tool to identify a dural hematoma. Also, in most cases, a hematoma, if present, is easily seen on a CT scan of the brain. Compared with other brain imaging techniques such as cranial MRI or angiography, CT is preferred because of its high sensitivity, universality, can be performed quickly and is non-invasive.
On CT, an epidural hematoma can often be distinguished from a subdural hematoma by its biconvex appearance. Meanwhile, the subdural hematoma has a crescent shape and shows a contour along the cerebral sulcus. Even so, if the epidural hematoma is small, it may be difficult to distinguish it from a subdural hematoma. Simultaneously, at the same site on the brain, both epidural and subdural hematomas can be present.
In addition, the density on the CT film of the hematoma also helps the doctor determine when the hematoma occurs.
Acute hematoma: High intensity. Blood clots can also be observed. Subacute hematoma: Homogeneous attenuation when bleeding has stopped Chronic Hematoma: Decreased attenuation due to clot dissolving and reabsorption. Occasionally, calcification of the dura is seen at the site of the hematoma. In addition, many repeat CT scans will help assess the progress of the blood mass and plan interventions as well as other brain injuries, especially signs of brain compression, brain herniation.
Ngoài chụp CT, có thể chụp MRi để chẩn đoán máu tụ ngoài màng cứng
4. How to treat epidural hematoma?
If a recent head injury occurs and an epidural hematoma is confirmed, this is always an emergency. Treatment goals include:Take measures to resuscitate, maintain life when circulatory and respiratory functions are threatened, control symptoms, minimize or prevent permanent damage to the parenchyma Brain One of the measures to help ensure the patient's life when a subdural hematoma is diagnosed, especially in the context of a rapidly developing and rapidly developing hematoma, is emergency surgery. This intervention is needed to help reduce pressure in the brain. The doctor may proceed by drilling a small hole in the skull to relieve pressure and allow blood to flow out of the skull. If the hematoma is large or there is a blood clot, the condition needs to be removed through a larger craniofacial opening in the skull. The skull cap will be closed with another surgery when the patient's condition is stable.
Besides, medical treatment with drugs will be used in addition to surgery depending on the degree of hematoma and the severity of symptoms as well as sequelae of brain damage. Among them, antiepileptic drugs may be used to control or prevent seizures due to secondary epilepsy. For these situations, epilepsy treatment can be lifelong.
5. What are the prognosis and complications after epidural hematoma?
Dural hematoma will have a high risk of death if not promptly surgical intervention. Even with early intervention, the risk of death or subsequent disability remains. Even if the dural hematoma has been treated, seizures can still occur. In some cases, seizures can occur up to two years after the injury.Other complications after dura Sensation of a part of the body Memory loss or loss of concentration In summary, a dural hematoma is a major neurological event following traumatic brain injury. As soon as a fall in the head is detected, it is necessary to quickly bring the patient to the hospital for a CT scan to diagnose skull damage and identify dural hematoma. When an epidural hematoma is identified as early as possible, early intervention improves long-term outcomes. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and hospital treatment.
With more than 14 years of working in the field of BSCK II imaging, Khong Tien Dat is currently a radiologist at Vinmec Ha Long International Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
How dangerous is a subdural hematoma after an injury? Chronic subdural hematoma in the elderly Subdural hematoma: Symptoms, diagnosis and treatment