This is an automatically translated article.
The article was written by MSc Nguyen Van Huy - Emergency Department - Vinmec Ha Long International HospitalTo confirm the diagnosis of skull and craniocerebral injuries, doctors will give patients a skull X-ray and a computed tomography scan of the brain for diagnosis. After an accident or trauma, if a patient has any of the following symptoms, they must go to the Emergency Department immediately.
III. Early lesions occur immediately after traumatic brain injury
1. Symptoms of a traumatic brain injury Unconsciousness or excessive somnolence, Continuous vomiting, Severe headache or dizziness that gets worse and worse, Convulsions, fainting or spasms face or limb, Unusual behavior or confusion, Difficulty waking up, Arms or legs becoming weak, Abnormal or unsteady gait, Slurred speech, Blurred or double vision, Hemorrhage from the ear or nose. In most cases, if a patient is concerned about any of the symptoms, the patient's family or friends should not delay but take the patient to see a doctor immediately.Pay special attention to cases of early traumatic brain injury in children, sometimes difficult for examination and evaluation. In the case of a head injury, if you see a child with one of the following signs, parents need to take the child to the hospital immediately.
Immediately after the fall, the child was unconscious for more than 1 minute. Immediately after the fall, the child is still awake, but after a while, abnormal cognitive signs appear (difficulty agitation, sleep a lot, lethargy, poor contact or completely unconscious). After a head injury, the child vomits more than 5 times in a short time or vomits for more than 6 hours (which was normal before). The fontanelle of a child after a period of trauma is swollen, stretched, accompanied by a pale face. Children were injured in many places, there was a lot of bleeding.

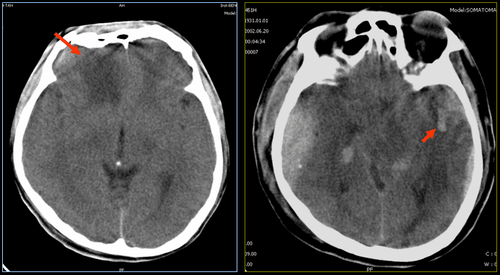
The common clinical picture is that immediately after the injury, the patient is still awake and then gradually goes into a coma, because the source of bleeding is the middle meningeal artery, so it is often acute, and coma and impaired consciousness. Rapid awakening due to the hematoma grows larger, requiring surgery to remove the hematoma, if the hematoma is quickly released, it will often improve clinical and prognosis. and usually the patient will be operated by the surgeon to remove the hematoma and reduce the intracranial pressure caused by the hematoma. The prognosis is usually quite good if the patient receives early, adequate, and staged intervention.
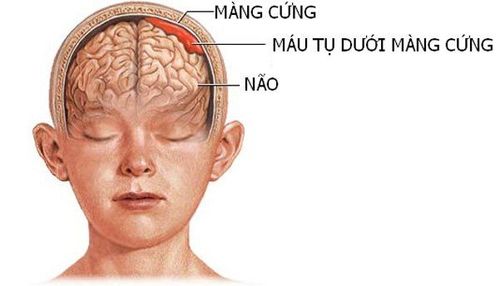
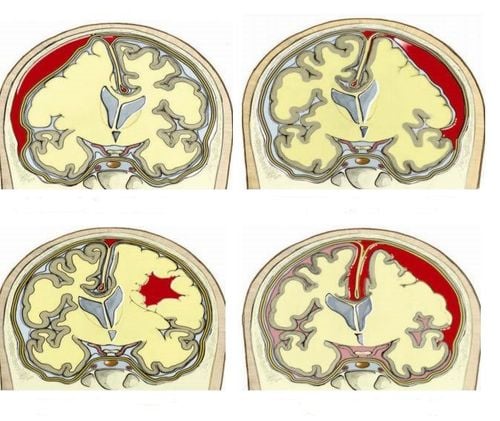
3. Subdural hematoma Subdural hematoma accounts for about 30% of all severe traumatic brain injuries. The injury often tears the vein bridge between the cerebral cortex and the veins draining the sinuses, conjuring brain tissue. This form usually develops slowly, because the source of bleeding is a tear in the cortical veins.
Therefore, it rarely appears in the first place, although in fact there are still cases of patients with subdural hematoma immediately after traumatic brain injury.
On computed tomography (CT) of the brain, there is a crescent-shaped hematoma, which can be combined with signs of cerebral contusion and subarachnoid hemorrhage, other cerebral edema, and subdural hematoma. 80% progression and prognosis of severe traumatic brain injury.
4. Intracranial hematoma Intracranial hematoma is common in moderate and severe traumatic brain injury, lesions are often in the frontal and temporal lobes, the hematoma may appear early or late. than on CT scan of the brain after 24 hours from the time of injury, so when the clinical worsens, it is necessary to repeat CT scan of the brain if traumatic brain injury is still suspected. The more foci of brain contusion, the worse the prognosis.
Diffuse axonal damage occurs very soon as soon as the trauma is usually caused by the impact of cutting the axon, causing swelling of the brain tissue, blocking the conduction and blocking the impulses. Traumatic injury causes axonal edema, which causes calcium ingress to damage cell membranes and mitochondria of axon cells, on the other hand, because damage in axons promotes programmed cell death.
This process has up to 50% role of axonal damage factors.
Diffuse axonal damage can cause disturbances of consciousness immediately after trauma, very high mortality, or prolonged vegetative state. This is one of the most severe injuries of traumatic brain injury, if there is axonal damage, it is almost irreversible and the mortality rate is very high.
Detecting axonal damage on CT scan of the brain is very difficult, can meet the images of lesions on computed tomography and magnetic resonance of the brain such as hemorrhagic dots and spots in the brain. border between white matter and gray matter which are essentially bleeding points due to axonal torsion, damage and rupture of CNS axons.
6. Concussion May be located just below the site of injury or opposite the site of the impact, usually in the forehead and temples. Brain contusion often has many foci, the brain contusion itself worsens consciousness if the pressure and cerebral edema increase.
In order to diagnose and monitor developments and intervene in a timely manner, we recommend patients who have been injured due to circumstances such as traffic accidents, work accidents, daily-life accidents, conflicts, Patients at risk of traumatic brain injury and other injuries must be monitored and treated in medical facilities to promptly detect and safely treat possible injuries.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.