This is an automatically translated article.
Article by Dr. Dr. Truong Ngoc Hai - Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Central Park International General HospitalThe frequency of reported plasma exchange-related complications (TPE) varies by definition and can be divided into 2 groups: infrequent procedure-related (17%) and adverse drug reactions. TPE is more common. Many recent studies have seen complication rates from 5 to 36%, most of which are mild and do not require intervention. Hypocalcaemia is most commonly associated with citrate anticoagulation in cTPE, less frequently in mTPE.
1. Complications of plasma exchange procedure
1.1 Electrolyte disturbances Citrate-associated hypocalcaemia is the most common complication in TPE because citrate is a common anticoagulant in the cTPE system and FFP is used as fluid replacement. Citrate binds with ionized calcium to form soluble calcium citrate, which reduces the serum concentration of ionized calcium. In patients with normal liver function, citrate is usually metabolized in about 1.5 hours. However, if the duration of TPE is prolonged, symptoms of hypocalcemia are likely to occur if not prevented. Common symptoms such as muscle twitching, numbness, paresthesia; more severe such as convulsions, QT prolongation, arrhythmias, hypotension. Therefore, in addition to reducing the rate of replacement, to limit hypocalcaemia, 10ml of 10% calcium chloride should be given slowly over 15-30 minutes after starting TPE 15 minutes and continued if the replacement is more than 1 hour, coordinate monitoring of electrocardiogram and ionized calcium test, especially those at risk of citrate toxicity (shock, liver failure), and patients who are unable to communicate to promptly report symptoms. early symptoms of hypocalcaemia (e.g. mental disturbances, children) [33].
Using a replacement fluid such as albumin can reduce blood potassium levels by 25% after TPE due to dilution so for people at risk of hypokalemia (poor diet, alkaline blood due to citrate), blood potassium should be checked. immediately after the procedure and adjust if necessary [49].
1.2 Hypotension Hypotension during or shortly after TPE is a common side effect accounting for approximately 20% of reported adverse events. In half of the cases, it is related to the extracorporeal circulatory system, in the remainder due to vagal or allergic reflexes [51].
Hypovolemia can occur when plasma is removed from the body and the replacement solution has lower or insufficient oncotic pressure leading to blood dilution causing a drop in blood pressure. This needs special attention because compared with hemodialysis the plasma volume in the TPE system is much larger. FFP contains a large amount of acid citrate dextrose causing actual protein concentration to be lower than plasma in the body, so care should be taken when performing high volume TPE with FFP, which can cause rapid decrease in oncotic pressure and circulatory volume causing hypotension. blood pressure. Insufficient volume replacement occurs if 5% albumin is used in patients with high blood albumin such as multiple myeloma. Therefore, the volume of fluid replacement should be calculated based on the patient's albumin and hematocrit, combined with monitoring of blood volume changes in TPE with devices such as the Crit-Line IV Monitor. When blood volume is decreased, it can be managed with: 25 % albumin infusion 20 ml/h, correction of albumin replacement levels, increased exchange rate (returned plasma/plasma fractionation ratio), bolus of sodium chloride. 0.9% 100–200 mL. It is important not to omit the fact that ongoing bleeding must be ruled out, especially in patients at high bleeding risk [51].
Decreased vascular resistance may be experienced by the vagus reflex when performing the needle puncture. In addition, in patients with autonomic neuropathies, the sympathetic system compensates incompletely and accurately and the decrease in vessel wall elasticity due to atherosclerosis is easy to cause hypotension during TPE. Besides, anaphylaxis with membrane system and FFP is a dangerous problem that needs to be detected and treated promptly [51].
1.3 Reactions to FFP Allergic reactions such as pruritus, urticaria can usually be treated by withholding TPE, administering diphenhydramine or glucocorticoids, and monitoring for signs of worsening. TPE may be restarted if symptoms are in remission. Allergic reactions such as urticaria are thought to be caused by preformed IgE antibodies in the recipient reacting to a substance in the donor or vice versa (eg, donor peanut allergy, hives). urticaria due to recent peanut consumption by the recipient) [8].
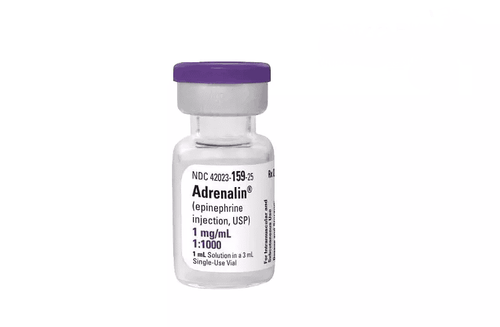
Anaphylaxis to plasma has been reported as a serious and potentially fatal complication of TPE. Management depending on symptom severity may include antihistamines, epinephrine, glucocorticoids, or more aggressive measures. In addition to the allergy-like mechanism mentioned, anaphylaxis may be due to the presence of anti-IgA antibodies in IgA-reactive hypo-IgA patients in the donor plasma. In cases of anti-IgA-induced anaphylaxis, plasma should be obtained from an IgA-lowering donor, but it may not be possible to obtain enough to perform TPE. Where this is not available, albumin should be used as a substitute or attempted desensitization using ephedrine, glucocorticoids, and diphenhydramine before TPE [8].
TRALI is an acute form of lung injury caused by antibodies in donor plasma that react with "related" or "matched" antigens on the patient's neutrophils, resulting in the cessation of leukocytes in the pulmonary circulation and cause noncardiac pulmonary edema. TRALI usually presents as sudden hypoxic respiratory failure, bilateral pulmonary infiltrates on chest radiographs during infusion or several hours after exposure to blood products. Treatment is mainly supportive, in severe cases the patient may need to be intubated [33].
1.4 Catheter involvement Complications of central venous catheters include pain, nerve damage, thrombosis, perforation, hematoma, air embolism or arteriovenous fistula, and infection. In the case of peripheral venous access, most of the complications associated with central venous catheterization can be avoided, but this is only relevant for cTPE with low blood flow, which increases TPE duration and may cause discomfort for the patient. Using internal ultrasound and checking for proper catheter placement is standard practice to limit some of these complications [49].
Catheter sepsis rates ranged from 0.6-6.5%/1,000 catheters/day, higher than in catheters used for dialysis and without cuff. Besides, the placement position greatly affects the infection rate: subclavian 5.1/1000 catheters/day, internal landscape 3.73/1000 catheters/day and 6.93/1000 catheters/day for venous catheters femoral pulse [51]. Therefore, careful evaluation is needed to detect early symptoms of catheter-related infection such as red, possibly pus-filled swelling at the site of insertion. Note the important points of catheter-associated sepsis: whenever sepsis is suspected, culture blood from the catheter tip and at least one external blood sample, culture the catheter tip; use empiric systemic intravenous antibacterial when dialysis catheter-associated sepsis is suspected, adjusted later according to the results of the antibiogram; Immediate removal of the infected catheter is the first choice of treatment.
2. Some research reports on plasma exchange complications
2.1 Research in the world Clinically, although TPE is used more and more widely, especially in critically ill patients, current studies only focus on evaluating the safety of TPE in a single patient. specific diseases and in dialysis departments, [14], [36], [38], [53]. There are relatively few studies evaluating the safety of TPE in critically ill patients. In addition, the lack of a unified definition of a complication and a reporting system caused the complication rate to vary widely across studies.
Author Lemaire did a prospective study on adult patients undergoing TPE at the HSTC department of Saint Louis University Hospital from January 1, 2013 to March 31, 2015 to evaluate the technical aspects and complications of the disease. TPE. The author enrolled 50 patients with 260 episodes of TPE: cTPE was the majority (61%) and both were equally effective in treating patients with hyperactivity syndrome. The rate of at least one complication was 26.9% and did not differ between the two separation methods. Among them, the most common complication is an allergy related to FFP. The authors also noted that hypotension was associated with low Hct before TPE and a 54% decrease in firbinogen after TPE when albumin was used as a substitute. Interestingly, the authors noted that membrane coagulation was not related to anticoagulation but could be related to a high volume of substitution, 4600 mL in the coagulation group compared with 3900 mL in the noncoagulated group, p < 0 ,01 [42].
Author Calça and his colleagues surveyed the HSTC department at Fernando Fonseca Hospital, Lisbon, Portugal, from January 2000 to April 2019 with 20 patients and 101 times of TPE, recording two common indications: depression muscle (25%), ANCA-associated vasculitis (15%). mTPE was performed using a Prismaflex, and Gambro with a central venous catheter. The mean number of TPE episodes per patient was 5.1±1.3 with replacement volumes between 2500-3500 mL with 5% albumin as the replacement fluid in 79.3%. The complication rate was 45.5%, mostly mild and transient, the most common were hypotension (6.9%) and hypocalcemia (4.9%) [12].
At Jagiellonian University Hospital, Cracow, Poland, Szczeklik investigated the prevalence of TPE-related complications in critically ill patients. With 370 episodes of TPE in 54 patients, he recorded common diseases for which TPE was indicated, including: myasthenia gravis (33.3%), Guillain-Barré syndrome (14%), Lyell's syndrome (9.3%). , SLE (7.4%) and TTP (7.4%). The most common adverse events were: hypotension (8.4%) arrhythmia (3.5%), cold feeling with transient increase in temperature and paresthesia (1.1%). In most cases, symptoms are mild and transient. Serious and life-threatening complications, such as shock, persistent hypotension requiring vasopressors, persistent arrhythmias, and hemolysis, occurred in 2.16% of TPE episodes [69].
2.2 Research in Vietnam Research by author Nguyen Minh Duc in 2017 on the effectiveness of treatment of Guillain - Barré syndrome by TPE method. After TPE, the symptoms were relieved at a very good and good level, the duration of the disease and the disease form both improved well. Changes in vital signs, laboratory tests before and after TPE were not significant; There were 26.3% of patients having complications and most of them occurred in the first time when performing the technique (18.0%), the most common were allergies (61.1%), other complications were unusual. is mild and does not affect the patient's life [2].
Author Le Quang Thuan studied the effectiveness of acute toxic hepatitis treatment at Bach Mai Hospital's Poison Control Center from January 2012 to December 2014 with 62 patients receiving active plasma exchange, compared with 52 patients. Patients in the historical control group in the period 2007-2011 received routine plasma exchange, which raised the prothrombin ratio above 40% and the total bilirubin concentration below 250 μmol/L, the mortality rate was 30.6%, reduced by 50%. risk of death compared with routine plasma exchange (61.5%). The author recorded that in 263 episodes of TPE, no complications were recorded in 77.9%, the most common complication was allergy accounted for 14.3%, in addition, there was 1 case of chills and 1 patient had anaphylactic shock. guard [5].
On patients resuscitated at Cho Ray Hospital, author Huynh Thi Thu Hien retrospectively reviewed patients who received TPE from January 2017 to June 2019 and recorded 78 patients with 121 TPE sessions, including 30 TPE times. - HV. The most common indications were acute liver failure and acute pancreatitis with hypertriglyceridemia, 54.5% and 27.3%, respectively. Common complications related to respiratory and allergic reactions with the rate of 5.8% and 5.0% of total TPE visits, respectively. For TPE-HV, the most common complication was respiratory complication (16.7%). The overall mortality rate in patients with acute liver failure was 23.1%, in which patients receiving TPE-HV had a mortality rate of 52.9% [3].
In our country, along with the development of dialysis technology in the wards of HSTC, mTPE is more and more widely used when it is possible to take advantage of the equipment and medical staff who are already familiar with supportive measures. extracorporeal support. However, current studies only focus on evaluating the effectiveness of TPE on a number of specific diseases, not accurately reflecting the situation of TPE indications at HSTC. In addition, the safety factor is only assessed together, which is mostly subjective records and lacks clear definitions. The study of author Huynh Thi Thu Hien initially recorded some indications and complications of TPE in resuscitated patients, we continue to further study this issue with changes in resuscitation practice. and the introduction of the latest ASFA recommendation 2019.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
TÀI LIỆU THAM KHẢO
Tiếng Việt:
Hoàng Đức Chuyên (2012), Nghiên cứu đặc điểm lâm sàng và điều trị viêm tụy cấp tăng triglyceride, Luận văn Thạc sĩ Y học, Trường Đại Học Y Hà Nội. Nguyễn Minh Đức (2017), Nghiên cứu đặc điểm lâm sàng, chẩn đoán điện và kết quả điều trị hội chứng Guillain – barré bằng phương pháp thay huyết tương , Luận văn Tiến sĩ Y học, Viện Nghiên Cứu Khoa Học Y Dược Lâm Sàng 108. Huỳnh Thị Thu Hiền (2020), "Liệu pháp thay huyết tương ở bệnh nhân nặng", Tạp chí Y Học Thành Phố Hồ Chí Minh , 24 (2), tr. 202-206. Thông Võ Duy (2021), “Tăng trirelycerie máu rất nặng ở bệnh nhân viêm tụy cấp: yếu tố nguy cơ và kết cục lâm sàng”, Tạp chí Y học Việt Nam , 2, tr. 49-55. Lê Quang Thuận (2017), Nghiên cứu hiệu quả điều trị viêm gan nhiễm độc cấp nặng bằng biện pháp thay huyết tương tích cực , Luận văn Tiến sĩ Y học, Viện Nghiên Cứu Khoa Học Y Dược Lâm Sàng 108. Võ Thị Đoan Thục (2020), Nghiên cứu hiệu quả của thay huyết tương trong điều trị viêm tụy cấp nặng do tăng triglyceride máu tại Bệnh viện Chợ Rẫy , Luận văn Chuyên khoa 2, Đại Học Y Dược Huế. Tiếng anh:
7. Ahmed S., Kaplan A. (2020), "Therapeutic Plasma Exchange Using Membrane Plasma Separation", Clin J Am Soc Nephrol , 15 (9), pp. 1364-1370.
8. Apter A. J., Kaplan A. A. (1992), "An approach to immunologic reactions associated with plasma exchange", J Allergy Clin Immunol , 90 (1), pp. 119-24.
9. Basic-Jukic Nikolina, Kes Petar, Glavas-Boras Snjezana, et al. (2005), "Complications of Therapeutic Plasma Exchange: Experience With 4857 Treatments". Therapeutic apheresis and dialysis : official peer-reviewed journal of the International Society for Apheresis, the Japanese Society for Apheresis, The Japanese Society for Dialysis Therapy , 9, pp. 391-395.
10. Beech C., Kumar D., Hendrickson J., et al. (2019), "Cryoglobulinemia as a Possible Primer for TRALI: Report of a Case". Lab Med, 50 (3), pp. 313-319 .
11. Bendapudi P. K., Hurwitz S., Fry A., Marques M. B., et al. (2017), "Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study", Lancet Haematol , 4 (4), pp. 157-164.
12. Calça Rita, Gaspar Ana, Santos Afonso, et al. (2020), "Therapeutic plasma exchange in patients in a portuguese ICU", Portuguese Journal of Nephrology & Hypertension , 34 (1), pp. 21-25.
13. Clebone A. (2019), "Transfusion reactions and cognitive aids". Curr Opin Anaesthesiol , 32 (2), pp. 242-246.
14. Colling M., Sun L., Upadhyay V., et al. (2020), "Deaths and complications associated with the management of acute immune thrombotic thrombocytopenic purpura", Transfusion , 60 (4), pp. 841-846.
15. Cordoba J. P., Larrarte C., Medina M. C. (2015), "Experience in therapeutic plasma exchange by membrane filtration at an academic center in Colombia: Registry of the first 500 sessions", J Clin Apher , 30 (6), pp. 347-52.
16. Daga Ruiz D., Fonseca San Miguel F., González de Molina F. J., et al. (2017), "Plasmapheresis and other extracorporeal filtration techniques in critical patients", Medicina Intensiva , 41 (3), pp. 174-187.
17. Erkurt M. A., Sarici A., Kuku I., et al. (2021), "The effect of therapeutic plasma exchange on management of HELLP Syndrome: The report of 47 patients", Transfus Apher Sci , 60 (5), pp. 1-3.
18. Evans L., Rhodes A., Alhazzani W., et al. (2021), "Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021 ", Intensive Care Med , 47 (11), pp. 1181-1247.
19. Fleischmann C., Scherag A., Adhikari N. K., et al. (2016), "Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations", Am J Respir Crit Care Med , 193 (3), pp. 259-72.
20. Fortenberry J. D., Nguyen T., Grunwell J. R, et al. (2019), "Therapeutic Plasma Exchange in Children With Thrombocytopenia-Associated Multiple Organ Failure: The Thrombocytopenia-Associated Multiple Organ Failure Network Prospective Experience", Crit Care Med , 47 (3), pp. 173-181.
21. Freireich E. J. (2011), "Leukocyte transfusion and the development of the continuous-flow blood cell separator", Transfus Med Rev , 25 (4), pp. 344-50.
22. Gajic O, Rana R., Winters J. L, et al. (2007), "Transfusion-related acute lung injury in the critically ill: prospective nested case-control study" . Am J Respir Crit Care Med, 176 (9), pp. 886-891.
23. Gashti C. N., Andreoli D. C., Patel D. (2018), "Membrane-based therapeutic plasma exchange (mTPE): Technical and clinical experience", J Clin Apher , 33 (1), pp. 38-45.
24. Guyton (2016), Guyton and Hall Textbook of Medical Physiology 13th , W B Saunders, Philadelphia, chapter 25, pp. 307-308 .
25. Hafer C., Kielstein J. T. (2017), "Pro: High dose of therapeutic plasma exchange-mind the gap!", Nephrol Dial Transplant , 32 (9), pp. 1457-1460.
26. Hafer C., Golla P., Gericke M., et al. (2016), "Membrane versus centrifuge-based therapeutic plasma exchange: a randomized prospective crossover study", Int Urol Nephrol , 48 (1), pp. 133-138 .
27. Hisamichi Mikako, Kawarazaki Hiroo, Oroku Masato, et al. (2016), "Risk factors for allergic reaction at initial therapeutic plasma exchange in a single-center study: beware of high rates of severe allergic reaction", Renal Replacement Therapy , 2 (1), pp. 2-5.
28. Horvatits T., Drolz A., Trauner M., et al. (2019), "Liver Injury and Failure in Critical Illness", Hepatology , 70 (6), pp. 2204-2215.
29. Hotchkiss Richard S., Moldawer Lyle L., Opal Steven M., Reinhart Konrad, Turnbull Isaiah R., et al. (2016), "Sepsis and septic shock", Nature Reviews Disease Primers , 2 (1), pp. 1-21.
30. Hu Lunyang, Wang Baoli, Jiang Yong, et al. (2021), "Risk factors for transfusion-related acute lung injury". Respiratory Care , pp. 08829.
31. Huang Y. K., Tan D. M., Xie Y. T., et al. (2012), "Randomized controlled study of plasma exchange combined with molecular adsorbent re-circulating system for the treatment of liver failure complicated with hepatic encephalopathy", Hepatogastroenterology , 59 (117), pp. 1323-1326.
32. Kandiah P. A., Olson J. C., Subramanian R. M. (2016), "Emerging strategies for the treatment of patients with acute hepatic failure", Curr Opin Crit Care , 22 (2), pp. 142-151.
33. Kaplan A. (2012), "Complications of apheresis", Semin Dial , 25 (2), pp. 152-158.
34. Kaplan A. A. (2013), "Therapeutic plasma exchange: a technical and operational review ", J Clin Apher , 28 (1), pp. 3-10.
35. Kes P., Janssens M. E., Bašić-Jukić N., Kljak M. (2016), "A randomized crossover study comparing membrane and centrifugal therapeutic plasma exchange procedures, Transfusion , 56 (12), pp. 3065-3072.
36. Khandelwal P., Thomas C. C., Rathi B. S., Hari P., Tiwari A. N., et al. (2019), "Membrane-filtration based plasma exchanges for atypical hemolytic uremic syndrome: Audit of efficacy and safety", J Clin Apher, 34 (5), pp. 555-562.
37. Kuldanek S. A., Kelher M., Silliman C. (2019), "Risk factors, management and prevention of transfusion-related acute lung injury: a comprehensive update", Expert Rev Hematol , 12 (9), pp. 773-785.
38. Kundrapu S., Datla S., Griffin V., Maitta R. W. (2019), "Adverse events during apheresis: A 10-year experience at a tertiary academic medical center", J Clin Apher , 34 (5), pp. 528-536.
39. Lahmer T., Messer M., Schnappauf C., Rasch S., Fekecs L., et al. (2017), "Impact of Therapeutic Plasma Exchange on Hemodynamic Parameters in Medical Intensive Care Unit Patients: An Observational Study", Artif Organs , 41 (2), pp. 204-209.
40. Larsen F. S., Schmidt L. E., Bernsmeier C., Rasmussen A., Isoniemi H., et al. (2016), "High-volume plasma exchange in patients with acute liver failure: An open randomised controlled trial" , J Hepatol , 64 (1), pp. 69-78.
41. Lee K. C., Stadlbauer V., Jalan R. (2016), "Extracorporeal liver support devices for listed patients", Liver Transpl , 22 (6), pp. 839-48.
42. Lemaire A., Parquet N., Galicier L., Boutboul D., Bertinchamp R., et al. (2017), "Plasma exchange in the intensive care unit: Technical aspects and complications", J Clin Apher , 32 (6), pp. 405-412.
43. Li Mao-Qin, Ti Jun-Xiang, Zhu Yun-Hang, et al. (2014), "Combined use of non-biological artificial liver treatments for patients with acute liver failure complicated by multiple organ dysfunction syndrome", World journal of emergency medicine , 5, pp. 214-217.
44. Lockwood C. M., Rees A. J., Pearson T. A., et al. (1976), "Immunosuppression and plasma-exchange in the treatment of Goodpasture's syndrome", Lancet , 1 (7962), pp. 711-5.
45. Mateen Farrah, Gastineau Dennis (2008), "Transfusion Related Acute Lung Injury (TRALI) after Plasma Exchange in Myasthenic Crisis". Neurocritical care , 8, pp. 280-282.
46. Meyer D. E., Reynolds J. W., Hobbs R., et al. (2018), "The Incidence of Transfusion-Related Acute Lung Injury at a Large, Urban Tertiary Medical Center: A Decade's Experience". Anesth Analg , 127 (2), pp. 444-449.
47. Miklaszewska M., Korohoda P., Zachwieja K., et al. (2017), "Filter Size Not the Anticoagulation Method is the Decisive Factor in Continuous Renal Replacement Therapy Circuit Survival", Kidney Blood Press Res , 42 (2), pp. 327-337.
48. Millar Jonathan E., Fanning Jonathon P., McDonald Charles I., et al. (2016), "The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology", Critical Care , 20 (1), pp. 387.
49. Mokrzycki M. H., Balogun R. A. (2011), "Therapeutic apheresis: a review of complications and recommendations for prevention and management", J Clin Apher , 26 (5), pp. 243-8.
50. Mortzell Henriksson M., Newman E., Witt V., et al. (2016), "Adverse events in apheresis: An update of the WAA registry data", Transfus Apher Sci , 54 (1), pp. 2-15.
51. Noiri Eisei (2014), “Complication”, The Concise Manual of Apheresis Therapy , Springer, Japan, chapter 17, pp. 177-224.
52. Padmanabhan A., Connelly-Smith L., Aqui N., Balogun R. A., Klingel R., et al. (2019), "Guidelines on the Use of Therapeutic Apheresis in Clinical Practice - Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue", J Clin Apher , 34 (3), pp. 171-354.
53. Palma-Garcia L., Velasquez-Rimachi V., Pezo-Pezo A., Roig J., Perez-Villegas J. (2018), "Therapeutic plasma exchange: Experience in a third level hospital, 2013-2016, Lima (Peru)" . J Clin Apher , 33 (4), pp. 480-485.
54. Paton E., Baldwin I. C. (2014), "Plasma exchange in the intensive care unit: a 10 year retrospective audit", Aust Crit Care , 27 (3), pp. 139-144.
55. Paugam-Burtz C., Levesque E., Louvet A., Thabut D., Amathieu R., et al. (2020), "Management of liver failure in general intensive care unit", Anaesth Crit Care Pain Med , 39 (1), pp. 143-161.
56. Puppe B., Kingdon E. J. (2014), "Membrane and centrifugal therapeutic plasma exchange: practical difficulties in anticoagulating the extracorporeal circuit", Clinical kidney journal , 7 (2), pp. 201-205.
57. Rajagopal K. (2019), "Left Ventricular Distension in Veno-arterial Extracorporeal Membrane Oxygenation: From Mechanics to Therapies", Asaio j , 65 (1), pp. 1-10.
58. Ranganathan Lakshmi, Menon Rema, Ramakrishnan Nagarajan, et al (2019), "Therapeutic Plasma Exchange Practices in Intensive Care Unit", Indian journal of critical care medicine , 23 (7), pp. 336-338.
59. Reeves H. M., Winters J. L. (2014), "The mechanisms of action of plasma exchange", Br J Haematol , 164 (3), pp. 342-51. .
60. Rimmer Emily, Houston Brett L., Kumar Anand, Abou-Setta Ahmed M., Friesen Carol, et al. (2014), "The efficacy and safety of plasma exchange in patients with sepsis and septic shock: a systematic review and meta-analysis", Critical care , 18 (6), pp. 699-699.
61. Roubinian N. (2018), "TACO and TRALI: biology, risk factors, and prevention strategies", Hematology Am Soc Hematol Educ Program , 2018 (1), pp. 585-594.
62. Sarode Ravi, Bandarenko Nick, Brecher Mark E., Kiss Joseph E., Marques Marisa B., et al. (2014), "Thrombotic thrombocytopenic purpura: 2012 American Society for Apheresis (ASFA) consensus conference on classification, diagnosis, management, and future research", Journal of Clinical Apheresis , 29 (3), pp. 148-167.
63. Schmidt J. J., Asper F., Einecke G., et al. (2018), "Therapeutic plasma exchange in a tertiary care center: 185 patients undergoing 912 treatments - a one-year retrospective analysis", BMC Nephrol , 19 (1), pp. 12.
64. Schwab P. J., Fahey J. L. (1960), "Treatment of Waldenstrom's macroglobulinemia by plasmapheresis", N Engl J Med , 263, pp. 574-9.
65. Sengul Samanci N., Ayer M., Gursu M., et al. (2014), "Patients treated with therapeutic plasma exchange: a single center experience"., Transfus Apher Sci , 51 (3), pp. 83-89.
66. Shumak Kenneth H., Rock Gail A. (1984), "Therapeutic Plasma Exchange", N Engl J Med, 310 (12), pp. 762-771.
67. Simetka O., Klat J., Gumulec J., Dolezalkova E, et al. (2015), "Early identification of women with HELLP syndrome who need plasma exchange after delivery", Transfus Apher Sci , 52 (1), pp. 54-59.
68. Stravitz R. Todd, Lee William M. (2019), "Acute liver failure", The Lancet , 394 (10201), pp. 869-881.
69. Szczeklik W., Wawrzycka K., Włudarczyk A., et al. (2013), "Complications in patients treated with plasmapheresis in the intensive care unit", Anaesthesiol Intensive Ther, 45 (1), pp. 7-13.
70. Toy P., Gajic O., Bacchetti P., et al. (2012), "Transfusion-related acute lung injury: incidence and risk factors", Blood , 119 (7), pp. 1757-67.
71. Tschope C., Ammirati E., Bozkurt B., Caforio A. L. P., Cooper L. T., et al. (2021), "Myocarditis and inflammatory cardiomyopathy: current evidence and future directions", Nat Rev Cardiol , 18 (3), pp. 169-193.
72. Vlaar A. P., Hofstra J. J., Determann R. M., et al. (2011), "The incidence, risk factors, and outcome of transfusion-related acute lung injury in a cohort of cardiac surgery patients: a prospective nested case-control study". Blood , 117 (16), pp. 4218-25.
73. Vlaar Alexander P. J., Toy Pearl, Fung Mark, et al. (2019), "A consensus redefinition of transfusion-related acute lung injury", Transfusion , 59 (7), pp. 2465-2476.
74. Wakelin Stuart, Janssens Michiel Etienne (2018), "Centrifugal and Membrane Therapeutic Plasma Exchange – A Mini-review", European Oncology & Haematology , 14 (2), pp. 105.
75. Wallace D. J. (1999), "Apheresis for lupus erythematosus", Lupus , 8 (3), pp. 174-180. .
76. Williams M. E., Balogun R. A. (2014), "Principles of separation: indications and therapeutic targets for plasma exchange" , Clin J Am Soc Nephrol , 9 (1), pp. 181-90.
77. Winters J. L. (2012), "Plasma exchange: concepts, mechanisms, and an overview of the American Society for Apheresis guidelines", Hematology Am Soc Hematol Educ Program , 2012 , pp. 7-12.
78. Yilmaz A. A., Can O. S., Oral M., et al. (2011), "Therapeutic plasma exchange in an intensive care unit (ICU): a 10-year, single-center experience", Transfus Apher Sci , 45 (2), pp. 161-166 .
79. Zhao Y., Garrity D., Graves M., Linden J., St Pierre P., et al. (2019), "Optimization of infusional calcium gluconate for prevention of hypocalcemic reactions during therapeutic plasma exchange" , J Clin Apher , 34 (6), pp. 656-660.