This is an automatically translated article.
People with diabetes are at risk of blindness many times higher than healthy people, because of diabetic eye complications such as cataracts, epidemic central retinitis, cataracts and especially cataracts. diabetic eye disease. The following article will detail the complications of diabetic eye fundus and some preventive measures.
Statistics of the World Diabetes Federation (IDF), in 2019 there were 463 million people with diabetes mellitus (diabetes). This is a chronic progressive disease that leads to dysfunction and failure of many organs in the body. Diabetes can cause many acute complications, increase the risk of infection, if long-term disease will affect large and small blood vessels. The complications that are easily seen in the heart, blood vessels, kidneys... are more commonly known. The silent but dangerous complication is vision loss leading to blindness that is easily overlooked. "On average, more than 50% of Asian patients, 70% in Vietnam, do not meet the treatment goal to bring blood glucose (HbA1c) below 7.0%, increasing the risk of eye complications."
1. What is diabetic eye disease?
Diabetic retinopathy, also known as diabetic retinopathy, damages the small blood vessels in the retina. The retina (also called the fundus) is the light-sensitive area of the eyeball, where nerve cells receive images to send to the brain for processing.At first, diabetic retinopathy may cause no symptoms or only mild vision problems. Finally, it can cause blindness.
This condition can develop in anyone with type 1 or type 2 diabetes. The longer you have had diabetes and the less controlled your blood sugar, the more likely you are to develop this eye complication. .
2.How diabetes affects the eyes The retina is the light-sensitive layer of cells in the back of the eye that converts light into electrical signals. Signals are sent to the brain and turn them into the images you see.
The retina needs a constant blood supply, which it receives through a network of small blood vessels. Over time, persistently high blood sugar can damage these blood vessels in 3 main stages:
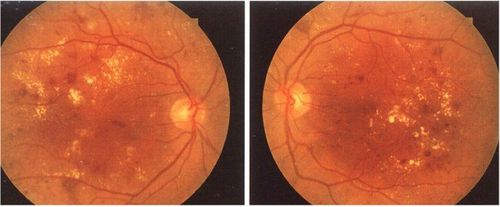
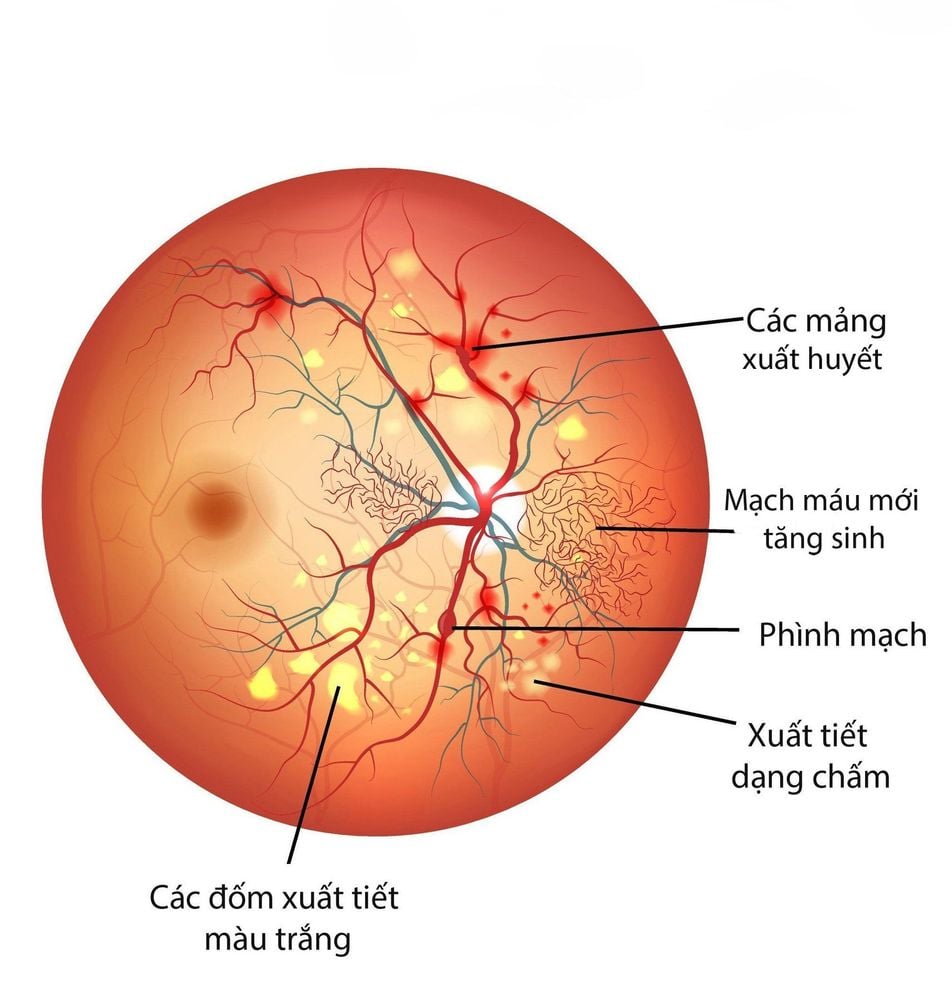
Background retinopathy (non-proliferative diabetic retinopathy (NPDR)) - new blood vessels don't grow development (proliferation). When you have NPDR, the walls of the blood vessels in your retina weaken. Small bulges (microaneurysms) protrude from the vessel walls of smaller vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels may begin to dilate and become irregular in diameter. NPDR can progress from mild to severe, as more blood vessels become blocked. Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macular) begins to swell (macular edema), a condition that requires treatment.
Pre-proliferative retinopathy - more severe and widespread changes affecting blood vessels, including more bleeding into the eye. Your vision may be affected. It is recommended to have a follow-up visit after 3 - 6 months to monitor your eye condition.
Proliferative retinopathy: Diabetic retinopathy can progress to a more serious type, called proliferative diabetic retinopathy. In this type, damaged blood vessels close, causing the growth of new, abnormal blood vessels in the retina and can leak into the jelly-like clear substance that fills the center of your eye (the vitreous). body). Eventually, scar tissue stimulated by the growth of new blood vessels can cause the retina to detach from the bottom of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build up in the eyeball. This can damage the nerve that transmits images from your eye to your brain (the optic nerve), leading to glaucoma.
However, if problems with your eyes are found early, lifestyle changes combined with treatment can prevent the condition from getting worse.
Bệnh võng mạc nền là một loại biến chứng mắt của đái tháo đường gây ra
3.Who is at risk for diabetic retinopathy? Anyone with type 1 or type 2 diabetes is at risk for diabetic retinopathy.
You are at higher risk if you:
Have had diabetes for a long time Have persistently high blood sugar (blood glucose) levels Have high blood pressure Have high cholesterol Are pregnant Are of Asian or African descent-Ca -riba By controlling blood sugar, blood pressure and cholesterol levels, you can reduce your risk of developing diabetic retinopathy.
4.Symptoms of Diabetic Retinopathy Usually you won't notice diabetic retinopathy in its early stages, as it doesn't tend to have any obvious symptoms until the disease is advanced. than.
However, early signs of this condition can be detected by taking pictures of the eyes during a diabetic eye exam.
Contact your doctor immediately if you experience:
Vision gradually worsens Sudden loss of vision Shapes floating in your vision Blurry or patchy vision Eye pain or redness These symptoms are not necessarily present This means you have diabetic retinopathy, but it's important that you get them checked.
5. Complications Diabetic Retinopathy Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications that can lead to serious vision problems:
Vitreous hemorrhage: New blood vessels may flow into the transparent jelly-like substance that fills the center of your eye. If the bleeding is small, you may see only a few dark spots (bumps). In more severe cases, blood can fill the vitreous and completely obstruct your vision.
Vitreous hemorrhage usually does not cause permanent vision loss. The blood usually clears from the eye within a few weeks or months. Unless your retina is damaged, your vision can go back to being as clear as before.
Retinal detachment: Abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This can cause floating spots in your vision, flickering of light, or severe vision loss.
Glaucoma: New blood vessels can grow in the front part of the eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye (glaucoma). This pressure can damage the nerve that carries images from your eyes to your brain (the optic nerve).
Blindness: Eventually, diabetic retinopathy, glaucoma, or both can lead to complete vision loss.

Các bệnh lý đáy mắt do đái tháo đường có thế gây mất thị lực hoàn toàn
6.How to check for diabetic retinopathy? Optometrists may check for diabetic retinopathy as part of a dilated eye exam. The exam is simple and painless - your doctor will give you some eye drops to dilate (widen) your pupils and then check your eyes for diabetic retinopathy and other problems. other eye problems or not.
If you have diabetes, it is important that you have regular eye exams. If you develop diabetic retinopathy, early treatment can stop damage and prevent blindness.
If your eye doctor thinks you may have severe diabetic retinopathy or DME, he or she may do a test called fluorescein angiography. This test allows your doctor to see images of the blood vessels in your retina.
After the examination the doctors will screen and give you an appointment as follows:
No retinopathy : Means no signs of retinopathy were found and you should attend the screening appointment followed by 12 months. Background retinopathy: Means you have stage 1 retinopathy and should attend your next screening appointment in 12 months. Degree of curable retinopathy: Means you have stage 2 or 3 retinopathy, or diabetic macular disease and should get tested more often or talk to a specialist about options treatment may be applied.
7.Treatment of diabetic retinopathy In the early stages of diabetic retinopathy, your ophthalmologist will likely just monitor the condition of your eyes. Some people with diabetic retinopathy may need regular comprehensive dilated eye exams every 2 to 4 months.
In the later stages, it is important to start treatment right away - especially if you experience vision changes. While it won't take away any damage to your vision, treatment can prevent your vision from getting worse. It is important that you take steps to control your diabetes, blood pressure, and cholesterol.
7.1. Treatment modalities 7.1.1. Laser treatment Laser treatment is used to treat new blood vessels at the back of the eye in the advanced stages of diabetic retinopathy. This is done because the new blood vessels tend to be very weak and often cause bleeding into the eye.
Treatment can help stabilize changes in your eyes caused by diabetes and prevent your vision from getting worse, although it usually doesn't improve your vision.
Laser treatment:
Involves shining a laser into the eye - you will be injected with a local anesthetic to numb the eye; Eye drops are used to widen your pupils and special contact lenses are used to keep your eyelids open and focus the laser on your retina Usually takes about 20-40 minutes Usually done on an outpatient basis, which means you won't need to stay in the hospital overnight May require more than one clinic visit for laser treatment, which is usually painless, although you may feel feel a stinging sensation when certain areas of your eye are being treated Possible side effects after treatment :
Blurred vision : You will not be able to drive until this has passed, so you need arrange for a friend or loved one to drive you home or take public transport Increased sensitivity to light : Wearing sunglasses may help until your eyes have adjusted Pain or discomfort : Pain relievers prescription, such as paracetamol. Possible complications:
Decreased night vision or peripheral (side) - some people may have to stop driving as a result of this Bleeding into the eye or floating objects in your field of vision Possible" see" laser-generated pattern on the back of your eye for several months A small, but permanent, blind spot near the center of your vision 7.1.2. Intraocular injections In some cases of diabetic macular disease, a medication called anti-VEGF can be injected directly into the eye to stop new blood vessels from forming at the back of the eye.
The main drugs used are called ranibizumab (Lucentis) and aflibercept (Eylea). These can help prevent your eye problems from getting worse and may also lead to an improvement in your vision.
During the treatment:
The skin around your eyes will be cleaned and covered with a towel Small forceps will be used to help widen your vision You will be given a local anesthetic to eye numbing A very small needle is carefully guided into your eyeball and injected The injections are usually given once a month to start. As your vision begins to stabilize, they will stop or become less frequent. Sometimes steroid injections can be used instead of anti-VEGF injections, or if anti-VEGF injections do not work.
Risks
Possible risks and side effects of anti-VEGF injections include:
Eye irritation or discomfort Bleeding inside the eye Sensation of something in your eye Watering or dry, itchy eyes There is also a risk that the injection could form a blood clot , which could lead to a heart attack or stroke . The main risk with steroid injections is increased pressure inside the eye.
7.1.3. Eye surgery Surgery may be done to remove some of the lens from the eye. This is a clear, jelly-like substance that fills the space behind the lens of the eye.
Surgery, called vitreous replacement surgery, may be needed if:
A large amount of blood has collected in your eye There is extensive scar tissue that is likely to cause or has caused retinal detachment During the procedure During surgery, the surgeon makes a small incision in your eye before removing some of the vitreous, removing any scar tissue, and using a laser to prevent further deterioration in your vision.
Vitreous surgery is usually performed under local anesthesia and sedation. This means you won't feel any pain or have any awareness of the surgery being performed.
After surgery:
You can go home the same day or day after surgery.
For the first few days, you may need to wear an eye patch. This is because activities like reading and watching television can quickly tire your eyes to begin with.
You may experience blurred vision after surgery. This should improve gradually, although it may take several months for your vision to return to normal.
Your surgeon will advise you on any activities you should avoid during your recovery
Risks:
Possible risks of cataract surgery include:
Develop cataracts Extra bleeding into the eye Retinal detachment Accumulation of fluid in the cornea (outermost layer at the front of the eye) Infection in the eye There is also a small chance that you will need retinal surgery add later. Your surgeon will explain the risks to you.

Phẫu thuật mắt là một trong những phương pháp hữu hiệu để điều trị các bệnh lý đáy mắt do đái tháo đường
8.Prevention of Diabetic Retinopathy You can't always prevent diabetic retinopathy. However, regular eye exams, good control of blood sugar and blood pressure, and early intervention for vision problems can help prevent serious vision loss.
If you have diabetes, reduce your risk of diabetic retinopathy by doing the following:
Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to get at least 150 minutes of moderate aerobic activity, such as walking, each week. Take your diabetes medication or insulin as directed. Monitor your blood sugar. You may need to check and record your blood sugar several times a day – it may be more frequent if you are sick or under stress. Ask your doctor how often you need to check your blood sugar. Ask your doctor about the glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood glucose level for the two to three months before the test. For most people, the A1C goal is less than 7 percent. Control your blood pressure and cholesterol. Eating healthy foods, exercising regularly, and losing excess weight can help. Sometimes medication is also needed. If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases the risk of various diabetes complications, including diabetic retinopathy. Pay attention to changes in vision. Contact your eye doctor right away if you have a sudden change in your vision or your vision becomes blurry, spotty, or hazy. Remember, diabetes does not necessarily lead to vision loss. Taking an active role in managing your diabetes can help you prevent complications in the long run.
To examine and treat eye diseases, you can go to the Eye specialist - Vinmec International General Hospital. The department has a comprehensive vision and eye health care function for children, adults and the elderly including refractive error testing, general examination, diagnostic ultrasound, laser treatment and surgery. In addition, ophthalmology also has the task of coordinating with other clinical departments in the treatment of pathological complications and eye injuries caused by accidents.
Why should you choose to examine and treat eye diseases at Vinmec International General Hospital?
Simple and quick procedure. Enthusiastic advice and support, reasonable and convenient examination process. Comprehensive facilities, including a system of clinics and consultations, blood collection room, dining room, waiting area for customers... The medical staff has high professional qualifications, style. Professional, caring way of working.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: nei.nih.gov