This is an automatically translated article.
Diabetes complications can lead to short-term and long-term health damage, including low blood sugar, heart disease, nerve damage and amputation, as well as vision problems. The majority of diabetic complications occur due to uncontrolled blood sugar levels, especially high blood sugar levels for a long time. The following article will introduce readers to common diabetes complications.
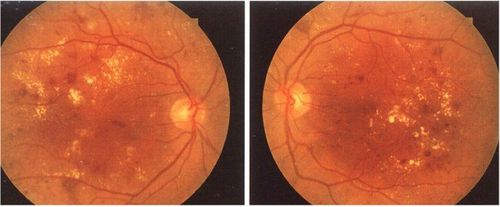
1. Diabetic retinopathy
Diabetic retinopathy is a complication of diabetes on the eye. It is also the most common cause of blindness in adults. The disease is characterized initially by retinal capillary microvascular lesions (background retinopathy) and then by neovascularization (proliferative retinopathy) and macular edema. Initially, the patient is usually asymptomatic, but then rapidly focal blurring, vitreous or retinal detachment; eventually partial or total loss of vision.
Screening and diagnosis of diabetic eye complications by retinal examination should be done regularly (usually annually) in both type 1 and 2 diabetic patients. Early detection and treatment of retinopathy Diabetic retinopathy is important for preventing vision loss, including aggressive blood sugar and blood pressure control. In addition, advanced retinopathy may require laser photocoagulation or, rarely, vitrectomy. Vascular endothelial growth factor inhibitors are also used for macular edema and as adjunctive therapy for proliferative retinopathy.
2. Diabetic kidney disease
Diabetic kidney disease is the leading cause of chronic kidney disease. This complication is characterized by thickening of the glomerular basement membrane, dilatation of the dermis, and glomerulosclerosis. The result is an increase in glomerular blood pressure and a gradual decrease in glomerular filtration rate. If the patient has concomitant systemic hypertension, progression may be accelerated. In most cases, there are no symptoms until nephrotic syndrome or chronic kidney failure develops.
Early diagnosis by yearly detection of albuminuria. The treatment of diabetic nephropathy is strict glycemic control combined with blood pressure control. ACE inhibitors or angiotensin II receptor blockers should be used to treat hypertension and, at the earliest signs of albuminuria, to prevent progression of kidney disease as these drugs lower blood pressure. glomeruli and thus have a protective effect on the renal filtrate.

Biến chứng tiểu đường có thể gây ra bệnh thận mãn tính
3. Diabetic Neuropathy
Diabetic neuropathy is a consequence of microvascular ischemic neuropathy, the direct effect of hyperglycemia on neurons, and intracellular metabolic changes that impair nerve function terrible.
This complication has many types but symmetric polyneuritis is the most common and affects the distal feet and hands, gloved distribution. Specifically, the patient has manifestations such as paresthesias, movement disorders or loss of painless sensation, vibration, sensation or temperature. In the lower extremities, these symptoms can lead to impaired perception of foot injury caused by ill-fitting shoes and abnormal weight, which in turn can lead to ulcers and infections of the foot or fractures, sprains, and fractures. tendon, dislocation, or destruction of normal foot structure (Charcot foot).
In addition, autonomic neuropathy belonging to the group of diabetic neuropathy is also common, which can cause orthostatic hypotension, resting tachycardia, dysphagia, nausea and vomiting, constipation, diarrhea, urinary incontinence, urinary retention, erectile dysfunction.
Treatment of diabetic neuropathy requires a multidimensional approach that includes glycemic control, regular foot care, and pain management. Tight blood sugar control can alleviate symptoms of neuropathy. Additionally, treatments to relieve symptoms include capsaicin topical cream, tricyclic antidepressants (eg, amitriptyline), serotonin-norepinephrine reuptake inhibitors (eg, duloxetine), and medications anticonvulsants (eg, pregabalin, gabapentin). Patients with loss of sensation should have their feet examined daily to detect a minor foot injury and prevent it from progressing to a life-threatening infection.
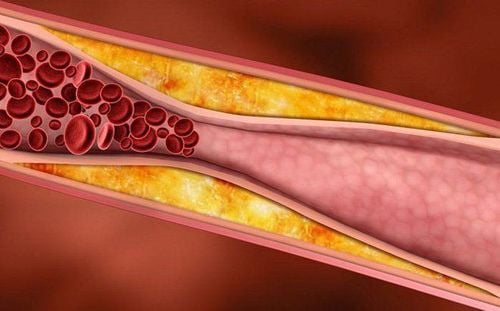
4. Major vascular complications
Large atherosclerosis is the result of long-term hyperinsulinemia, dyslipidemia and hyperglycemia - characteristic of diabetes, manifestations include:
Angina and myocardial infarction Attacks Transient ischemia and stroke Peripheral artery disease is a complication of diabetes in the legs or a complication of diabetes in the arms The diagnosis of diabetic macrovascular complications is made by history and physical examination. The course of treatment requires close control of atherosclerotic risk factors, including stabilization of plasma glucose, lipids, and blood pressure, combined with smoking cessation, daily aspirin and ACE inhibitors. . Furthermore, such a multifactorial approach is also effective in reducing long-term cardiovascular event rates.
Xơ vữa động mạch là một trong các biến chứng tiểu đường
5. Complications of cardiomyopathy
Diabetic cardiomyopathy is thought to be the result of multiple factors, including coronary atherosclerosis, hypertension and left ventricular hypertrophy, microvascular disease, endothelial dysfunction, obesity and metabolic disorders.
These patients often have heart failure due to impaired left ventricular systolic and diastolic function; at the same time is also prone to heart failure after myocardial infarction later.
6. Increased risk of infection
Patients with poorly controlled diabetes are more susceptible to bacterial and fungal infections because of the deleterious effect of hyperglycemia on granulocyte and T cell function.
In addition to an overall increase in risk Infectious diseases, people with diabetes are also susceptible to fungal infections of the skin and mucous membranes (eg, oral and vaginal candidiasis) and bacterial foot infections (including osteomyelitis). ), which is often aggravated by lower extremity vascular insufficiency and diabetic neuropathy. Furthermore, hyperglycemia is a well-defined risk factor for surgical site infection.
In summary, most people with diabetes usually begin to develop diabetes complications several years after having the disease. If you have good diabetes control and live a healthy, active lifestyle, you can avoid the risk of complications in the long run. Conversely, if blood sugar is not well controlled, has a less healthy lifestyle, or has undiagnosed diabetes, diabetes complications are more likely to develop earlier and progress rapidly. disability and reduced quality of life.
Currently, Vinmec has deployed a screening package for diabetes and dyslipidemia. Not only health screening, the diabetes and dyslipidemia screening package also helps to detect pre-diabetes early, accurately classify diabetes type, develop a nutritional regimen, and monitor the treatment of diabetes. risks and complications caused by diabetes. Especially with the expertise and science of a team of endocrinologists, they will examine accurately, methodically, advise and give useful advice to help diabetics live a happy, peaceful life. strong.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.