This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine, Vinmec Central Park International General Hospital
Patients who continue to have symptoms despite PPI therapy are considered to have refractory GERD, usually defined as the persistence of typical symptoms unresponsive to stable, twice-daily doses of PPIs. every day for at least 12 weeks of treatment. Up to 30% of GERD patients have treatment-resistant GERD.
Causes of failure of antacids (PPIs) with reflux esophagitis include:
8. Gastroesophageal reflux is not acidic
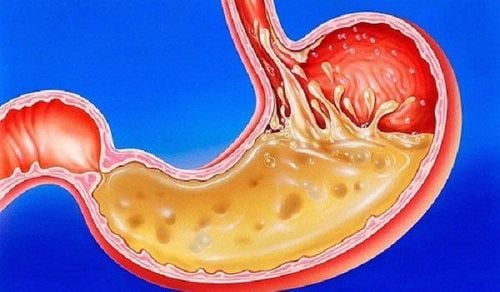
Non-acidic gastroesophageal reflux is the reflux of gastric contents into the esophagus with pH > 4. The introduction and recent use of multichannel endocardial impedance (MII) with sensing The pH variable allows detection of gastric reflux into the esophagus without simultaneously lowering the pH below 4. This recording cluster can reveal the characteristics of gastric reflux (gas, liquid, mixture). gas and liquid). By using MII with a pH sensor, Vela et al demonstrated altered reflux characteristics in patients with twice-daily PPI failure. Although there was no difference in the number of reflux cases on PPI treatment when compared with baseline, most reflux cases were found to be non-acidic. The authors suggest that nonacid reflux is associated with classic GERD symptoms, although less so than with acid reflux. Additionally, symptoms such as regurgitation, sour or bitter taste in the mouth are more related to non-acid reflux than heartburn. Shay et al evaluated 29 patients who were symptomatic despite twice-daily PPI treatment, using the MII‐pH test. Of the 22 patients who had symptoms on the study day, 41% had an abnormal MII but successful acid suppression and a positive symptom index (SI) for non-acid GER. Vomiting was the most commonly reported symptom (71%). In addition, 18% had both failed acid suppression and abnormal MII parameters, with symptoms related to acid reflux rather than to no acid. The remaining 41% had both successful acid suppression and normal MII. All those who were asymptomatic on the study day had a normal MII. This study showed that non-acid reflux was associated with symptoms in a small number of patients who failed PPI therapy.
The role of non-acid reflux, let alone its composition, in PPI failure remains to be elucidated. As with DGER, there is evidence for an association but the extent of causality is unknown. It is also unclear the extent of overlap between non-acid reflux and DGER.

9. Visceral hypersensitivity
As mentioned before, NERD contributes most of the people who do not meet PPI. Many of these patients originate from the functional heartburn subtype, which accounts for up to 50% of NERD patients.
Frazzoni et al recently evaluated patients with different phenotypic manifestations of GERD (NERD, erosive esophagitis, and complex GERD) and compared them with patients with functional heartburn. Patients with functional heartburn were not different in the history of acid exposure in the distal esophagus, the incidence of diaphragmatic hernia, distal esophageal spasm, and basal subesophageal sphincter (LES) pressure compared with the control group. normal symptoms. This study further demonstrates that mechanisms other than reflux are likely to play an important role in symptom generation in people with functional heartburn. Martinez et al. demonstrated that patients with NERD and an abnormal pH test were more likely to demonstrate an SI > 75% than patients with functional heartburn (61.9% vs 10.5%, P=0.001). . In the functional heartburn group, those with a negative SI reported heartburn at pH <4 only 12.7% of the time compared with 70.7% of the time in those with a positive SI, despite the average number of heartburn episodes. similar jar. Therefore, the authors propose that most (63%) patients with functional heartburn present with heartburn symptoms unrelated to acid reflux. However, the authors also suggested the presence of a subgroup of patients with functional heartburn and demonstrated a close relationship between their heartburn symptoms and acid reflux events. Further support for this subgroup of patients stems from a treatment study in patients with functional heartburn who received a twice-daily PPI. In this study, the authors demonstrated that partial response to PPI therapy in patients with functional heartburn could be due to subgroups of patients demonstrating a strong correlation between their symptoms and acid reflux events.
To date, the mechanisms of pain in patients with functional heartburn appear to be diverse, and acid exposure in the physiological range is the underlying cause in only a small subset of patients. However, repeated studies in patients with functional heartburn, using balloon esophagectomy or electrical stimulation have consistently demonstrated a threshold for pain when compared with those with pain. patients with other GERD manifestations. Furthermore, objective neurophysiological measures of esophageal evoked potential latency suggest that functional heartburn patients achieve comparable latency and amplitude evoked esophageal potential response to head decreased afferent, indicating increased esophageal sensitivity.
In contrast, acid-responsive functions in functional heartburn patients showed a more mixed response, leading to a higher mean time to heartburn and a mean averages were lower in perfusion intensity and sensitivity scores when compared with patients with NERD and test abnormal pH. One-quarter of the patients had negative acid infusion test results. The second study further supports the hypothesis that functional heartburn develops in a heterogeneous group of patients. However, a substantial subgroup of these patients did not have GERD as the underlying trigger for their heartburn. Further research is needed to explore different mechanisms for symptoms in patients with functional heartburn, including the possibility of small changes in esophageal pH that are not consistent with pH 4.0. arbitrary definition for the acid reflux event). It is unlikely that GERD symptoms will be produced only if the pH drops below 4.0. In addition, there are emerging data showing that even minute changes in esophageal pH are sufficient to induce heartburn symptoms in a small subset of patients with GERD.
10. Empty the stomach
Delayed gastric emptying is generally considered to be an important contributing factor to the pathophysiology of GERD. Several studies have demonstrated that the rate of delayed gastric emptying in patients with GERD is about 40%. Some researchers have recognized that delayed gastric emptying may contribute to PPI failure in patients with GERD. Kudara et al. Evaluation of gastric emptying in 15 patients with erosive esophagitis receiving lansoprazole 30 mg once daily for 8 weeks. Four of the patients who experienced persistent reflux symptoms and erosive esophagitis demonstrated significantly slowed gastric emptying when compared with 11 other patients who had improved GERD symptoms and esophagitis. manage.
To date, there are few data on the frequency of delayed gastric emptying in patients who have failed PPI therapy. It is well known that patients with diseases that cause delayed gastric emptying do not demonstrate a higher incidence of erosive esophagitis. In addition, there was no correlation between delayed gastric emptying and response to PPI therapy.
Regardless of the extent and role of delayed gastric emptying in patients with PPI failure remains to be elucidated. It is possible that patients may continue to report this type of dyspepsia during PPI treatment. These symptoms can be confused and related to PPI failure.
11. Mental illness
Other factors that can lead to PPI failure, such as psychosocial comorbidities, emotional status, and stress have never been evaluated. These factors appear to play an important role in patient compliance as well as response to treatment.
12. Conclusion
GERD resistant to PPIs is a common problem affecting a large proportion of patients with GERD. Resistant GERD may not have an underlying cause and may actually represent several disease states. Potential causes include drug nonadherence, visceral hypersensitivity, non-acid reflux, motility disturbances, and altered PPI metabolism. Other disease states such as achalasia, EoE, and esophageal cancer must also be considered. The primary basis for evaluating a patient with refractory GERD is upper gastrointestinal endoscopy and impedance monitoring to clarify the nature of any undetermined reflux cause.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
F. Fass , M. Shapiro , Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease – where next? Alimentary Pharmacology and Theurapeutics, Volume22, Issue2, July 2005 Vaezi MF. ‘Refractory GERD’: acid, nonacid, or not GERD? Am J Gastroenterol 2004; 99: 989– 90. Richter JE, Bochenek W. Oral pantoprazole for erosive esophagitis: a placebo-controlled randomized clinical trial. Pantoprazole US GERD Study Group. Am J Gastroenterol 2000; 95: 3071– 80. Please refer to the following sections:
Causes of failure of antacids (PPIs) with reflux esophagitis (Part 1) Causes of failure of antacids (PPIs) with reflux esophagitis (Part 2) Causes of failure of antacids (PPIs) with reflux esophagitis (Part 3) Causes of failure of antacids (PPIs) with esophagitis Reflux Management (Part 4)