This is an automatically translated article.
The article is professionally consulted by Resident Doctor, Master Nguyen Van Anh - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International Hospital
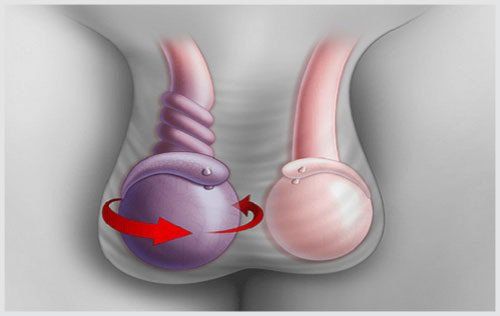
Ultrasound diagnosis of testicular trauma can reliably assess scrotal lesions and testicular rupture with high accuracy. Ultrasound can provide important information regarding testicular perfusion, adding additional diagnostic information before making decisions regarding surgery.
Injuries to the penis and testicles are uncommon, but when they do, they often lead to serious complications. Early complications include testicular infarction, necrosis, and abscess formation; After trauma, testicular atrophy and infertility can occur. Early surgical intervention in patients with testicular trauma can significantly improve clinical outcomes and reduce the need for late-stage orchiectomy. However, clinical examination of the scrotum after trauma is difficult and often inaccurate; This may lead to incorrect patient classification for surgical exploration.
1. What is testicular trauma?
Trauma to the testicles is an uncommon urogenital system injury, accounting for less than 1% of cases. The mechanism of injury is usually due to pressure between the legs or traumatic force between the pubic joint and a hard surface, especially during sports.
Testicular trauma is usually unilateral. Two testicles convulsion usually accounts for only about 2%. Trauma usually occurs in men between the ages of 15 and 40.
Based on the cause, testicular trauma is divided into 2 groups:
Closed testicular trauma: That is, the testicle is injured but the skin of the scrotum is Still intact or only slightly scratched. Patients often have closed testicular trauma during sports or traffic accidents. The most common form of trauma is a hematoma in the testicle, which ruptures the testicle tissue, causing the testicle to swell and become painful. Open testicular trauma: Testicular trauma accompanied by open wounds, communicating with the outside environment. The cause of testicular trauma in this case can be a weapon such as a knife, bullet, explosive, animal bite. Trauma to an open testicle often causes significant blood loss and increases the risk of infection. Based on anatomy, testicular trauma is classified into:
Bleeding in the testicular parenchyma, forming hematomas causing painful swelling of the testicle. The white capsule ruptures, causing the testicular parenchyma to overflow under the scrotal layers, creating a hematoma in a shallower location. Hemorrhage under the visceral peritoneum. Rupture of small blood vessels under the skin.

2. Clinical recognition of testicular trauma
Injury to the testicles, though uncommon, is troublesome and can have serious consequences for the patient. After trauma, people with testicular trauma often experience sharp pain in the scrotum, accompanied by swelling, testicles increase in size.
The degree of swelling of the scrotum has no direct correlation with the degree of testicular trauma. If the parietal lamina is preserved, blood and testicular parenchyma will be localized, so that clinically there is no significant difference between the injured and healthy scrotum. During clinical examination, it is difficult for the doctor to palpate the damaged testicle because it is located deep in the hematoma and tissue damage, the patient feels very painful, hindering the examination.
When there is a hematoma and tissue contusion of the testicle, the blood vessels supplying the testicle are compressed, causing the blood circulation to nourish the testicles. Complications of testicular trauma are testicular infarction, testicular necrosis, and testicular atrophy. Some cases of acute anemia can cause the skin of the scrotum to turn purple and pale. The purple patch may spread to the opposite side and up to the lower abdomen.
3. Can ultrasound detect testicular trauma?
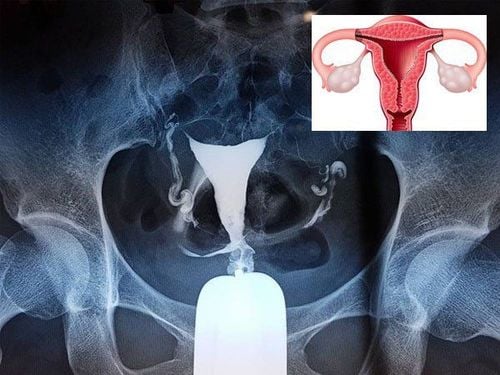
Ultrasound is the first imaging tool when approaching the diagnosis of scrotal trauma in general and testicular trauma in particular. Clinical manifestations are not always reliable. Clinical features do not help diagnose or rule out disease, nor do they correlate with the severity of testicular trauma. Moreover, the patient is often very painful, so the clinical examination is often not going smoothly.
Testicular trauma images obtained on testicular ultrasound are often characterized by mixed echogenicity, heterogeneity, and white capsule rupture. On doppler ultrasound of the testicles, poor perfusion was obtained.
Mixed echogenic structures in testicular trauma appear when the testicular parenchyma is contusionally damaged. When the impact force is strong enough, the white bag can be broken. White capsule tears are detected on ultrasound based on the loss of continuity. However, if the hematoma is subcutaneous, the white capsule surrounding it is too large to interfere with the reception of the ultrasound signal. The combination of many features on ultrasound can help increase the accuracy in diagnosing testicular trauma, especially testicular rupture.
Decreased or lost blood circulation to the testicles on ultrasound varies depending on the extent of the injury. Testicular perfusion helps to identify healthy tissue and predict the ability to preserve testicular parenchyma. If the hematoma is large, causing compression leading to decreased perfusion of testicular tissue, emergency surgical removal of the hematoma should be performed to preserve reproductive function of the testicle.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.