This is an automatically translated article.
The article was professionally consulted by Bachelor Tran Hue Tran - IVF Specialist - Reproductive Support Center - Vinmec Times City International Hospital.Semen analysis (semen analysis) is an important test in male reproductive health examination. This test indicates the sperm count and the quality of the sperm. Through it, the doctor can assess a man's ability to conceive during normal sex.
1. Semen analysis
1.1. What is semen analysis?
Semen analysis is a test that evaluates the quality of sperm, through indicators such as count, motility, normal shape...You should also tell your doctor about any medications or any herbal supplements you are taking. Drugs that can affect your test results include:
Testosterone: These hormone-boosting supplements can send the wrong signals to your body and cause your body to stop producing testosterone and natural sperm. It can lead to low sperm count. Anabolic steroids: These are used to strengthen muscles, these drugs can affect how your body produces sperm. Marijuana: The THC (tetrahydrocannabinol) in marijuana can lower your sex drive and prevent your body from making testosterone and sperm as it should. Opioids: These can lower sperm count and affect testosterone production. To get the most accurate results, your doctor will recommend that you do this test 2 or more times. You will need to provide another sample within 2 to 3 weeks after the first test. This is because semen samples from the same man can vary. You may even need to provide two to three samples over a 3-month period.
1.2. Why analyze semen?
If you and your partner are having trouble getting pregnant, one of the first tests your doctor will likely order is a semen analysis.Male infertility accounts for about 30% of infertility causes, of which more than 90% are due to sperm abnormalities. Abnormal sperm production or function.
Another reason you may need a semen analysis is to make sure that a vasectomy (a procedure to prevent pregnancy) was successful. This is usually done 8 to 16 weeks after surgery to see if there are still healthy sperm in your semen.

Phân tích tinh dịch giúp bác sĩ đánh giá chất lượng tinh trùng nam giới
1.3. Prepare for semen analysis
Before checking your semen, the doctor will give complete and detailed instructions to get the best sperm sample:Time to abstain from ejaculating before sampling is 2-7 days. Collect semen by masturbation (in case masturbation is not possible, a specialized condom can be used for intercourse) Ejaculate directly into a dedicated sample container. In case it is not possible to collect samples at the hospital, samples can be collected at home. Samples must be recorded at the time of ejaculation, stored at a temperature of about 20 - 37oC and immediately transferred to the laboratory within 1 hour from the time of ejaculation. Do not use lubricants as lubricants often contain spermicide, which can affect the results. Semen analysis (semen analysis) is an important test in a male reproductive health exam. This test indicates the sperm count and the quality of the sperm. Through it, the doctor can assess a man's ability to conceive during normal sex.

Một số loại thuốc có thể ảnh hưởng đến chất lượng tinh trùng của nam giới
2. Normal sperm count
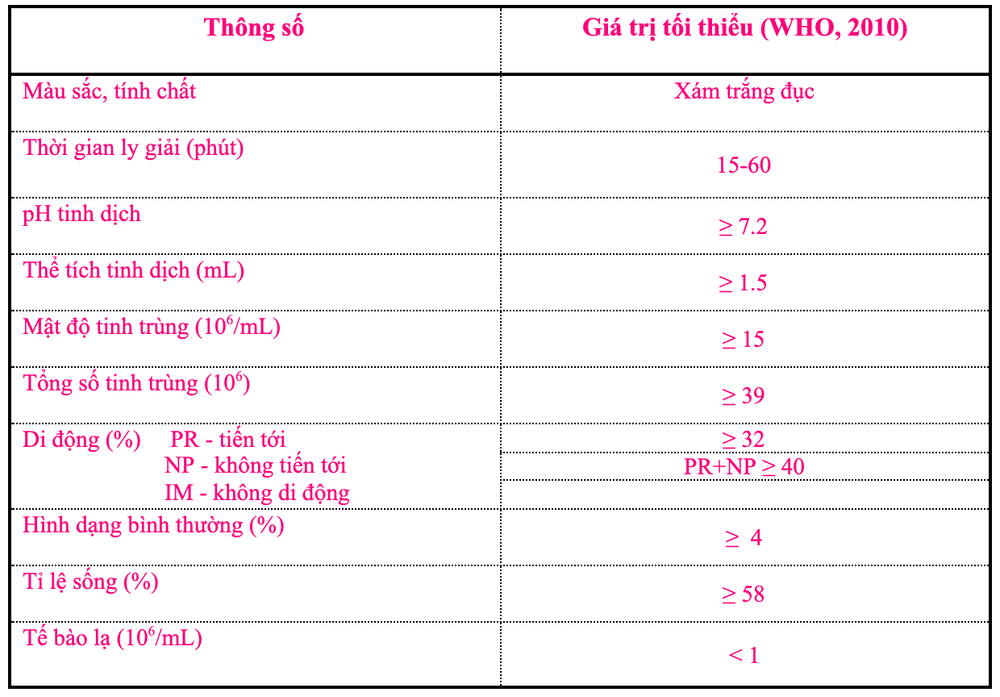
Normal sperm count: ≥ 15 million sperm per milliliter (mL) of semen and total sperm count ≥ 39 million. If the sperm count is less than 15 million per milliliter, or less than 39 million sperm per ejaculation, it is considered low and is called oligospermia.Semen analysis, in addition to checking the sperm count, also shows the shape of the sperm and the movement of the sperm or the motility of the sperm.
Sperm count, shape and motility are important to evaluate male factor infertility. Your doctor may recommend testing up to three sperm samples at different visits for accurate analysis.
Table of semen analysis results according to the minimum standards of the World Health Organization (WHO), 2010.
3. Why is sperm count important?
If you are trying to conceive naturally, a healthy sperm count is often essential. Although only one sperm fertilizes one egg to form an embryo, having more healthy sperm increases your chances of getting pregnant each month.Even if you're not trying to conceive, your sperm count can be an important gauge of overall health. One study found that men with a low sperm count were more likely to experience the following problems than men with a higher sperm count:
Higher percentage of body fat with larger waist circumference and a higher BMI. Higher blood pressure. High risk of metabolic syndrome Diabetes. Heart disease. So if you're diagnosed with a low sperm count, your doctor may want to evaluate your testosterone levels, lifestyle, and overall health.

Nam giới mắc bệnh lý tim mạch có khả năng số lượng tinh trùng thấp hơn người bình thường
4. How does sperm count affect fertility?
Sperm count can affect your ability to conceive, as your partner's chances of getting pregnant decrease when the sperm count is lower. Problems with sperm quality can also affect fertility.Male infertility often comes from low sperm count, this is also a common reason why many couples have difficulty conceiving. But couples can also experience other health problems that affect fertility.
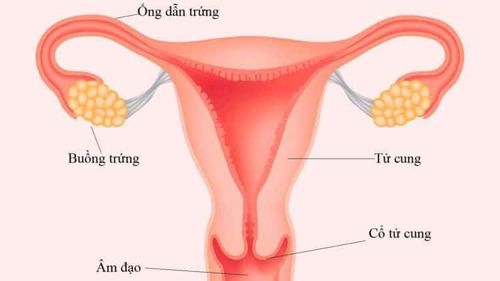
Low ovarian reserve A blocked fallopian tube Endometriosis Failed conception can also be the result of not trying to conceive long enough. In many cases, it can take six months to a year to get pregnant when there are no fertility problems.
If you are over 35 and you have been trying to conceive for six months, your doctor may refer you to a fertility specialist. If you've been trying to conceive for more than a year and both you and your partner are under 35, see your doctor for advice.
There are many factors involved in reproduction, and the sperm count in your semen is only a fraction of them. Some men have a low sperm count but still have normal fathers. Meanwhile, some men have normal sperm counts but are unable to father children. Even if you have a sperm count, other factors are important for getting pregnant, including normal sperm movement.
Depending on the initial exam and test results, your doctor may recommend additional tests to look for the cause of low sperm count and other possible causes of male infertility. These may include:
Testicular ultrasound : this test uses high-frequency sound waves to look at the testicles and supporting structures. Hormone tests: Your doctor may recommend testing the levels of hormones produced by the pituitary gland and testicles, which play an important role in sexual development and sperm production. Post-ejaculation urinalysis: the presence of sperm in your urine may show that your sperm is going back into the bladder instead of out through the penis during ejaculation. Genetic tests: when sperm concentration is extremely low, genetic factors may be the cause. Blood tests can show whether there are small changes in the Y chromosome that are indicative of a genetic abnormality. This test may also be ordered to diagnose various congenital or inherited syndromes. Testicular biopsy: This test involves taking a sample from the testicle with a needle. This test can tell if sperm production is normal. If sperm production is normal then your problem could be caused by a blockage or another problem in sperm transport. However, this test is usually only used under certain circumstances and is not commonly used to diagnose the cause of infertility. Anti-sperm antibody tests: This test is actually not very common. These tests are used to check for immune cells (antibodies) that attack the sperm and affect its ability to function. Specialized sperm function tests: Some tests may be used to check how well sperm survive after ejaculation. These tests can assess how well the sperm is getting into the egg and whether there is a problem attaching to the egg. Transrectal ultrasound: A small lubricated ultrasound probe is inserted into the rectum to check for the prostate gland and blockage of the seminal ducts.

Siêu âm tinh hoàn có thể được bác sĩ lựa chọn giúp tim nguyên nhân gây vô sinh nam
5. Is there any treatment for low sperm count?
Many studies have shown that low sperm count can be caused by a number of factors, including:Genetic factors Past surgery Overall health Sexually transmitted diseases Treatment options Low sperm count conditions may include:
Surgery: if you have varicocele or blocked vas deferens, you should have surgery to correct these conditions. Antibiotics: if a bacterial infection is affecting sperm count or fertility, your doctor may prescribe antibiotics. Medications or psychotherapy: they can be used for sex problems like erectile dysfunction or premature ejaculation. Medications and hormone treatments: For cases where high or low hormone levels affect infertility, hormone treatments can be helpful.
6. Improve sperm count
In addition to a few causes of low sperm count that require medical intervention, you can completely improve your own sperm quality by making lifestyle changes. The following things can improve sperm count:Lose weight: if you are obese or overweight that can cause low sperm count. Trying to maintain a healthy lifestyle through diet and exercise can help increase sperm count. Take a vitamin supplement: Your doctor may recommend that you have a blood test to check for a vitamin deficiency. Your doctor may recommend adding new foods to your diet or taking supplements to help restore needed vitamin and mineral levels. Do not use stimulants, including heavy drinking and drug or tobacco use. Wear comfortable clothing Many factors affect your sperm count, including lifestyle or underlying medical conditions. If you have a low sperm count, your doctor can suggest options for you to increase your sperm count, or advise you to see a urologist or fertility specialist, if needed.
If you have a low sperm count and you are trying to conceive, there are many options available to help you conceive today, including a range of treatments such as:
Intrauterine insemination (IUI) ) In vitro fertilization (IVF) IVF with intracytoplasmic sperm injection (ICSI) Most importantly, you and your partner need to see a specialist for advice and instructions on eating, drinking, Use medications that are most appropriate for your current health condition.

Trung tâm Hỗ trợ sinh sản - Bệnh viện Đa khoa Quốc tế Vinmec được nhiều cặp vợ chồng lựa chọn thăm khám
Thanks to the good quality of examination and modern facilities, the hospital has helped many couples realize their dream of becoming parents in the near future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: healthline.com - webmd.com - mayoclinic.org