This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
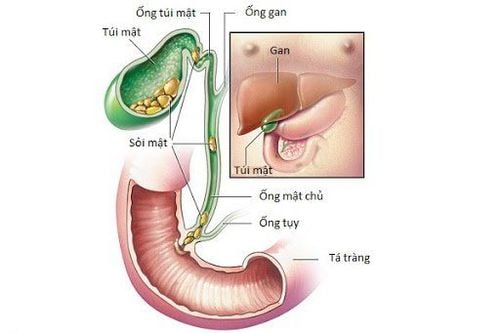
Cholescintigraphy is performed by nuclear medicine physicians as tests to diagnose biliary tract obstruction (eg, by gallstones or tumors), gallbladder disease, and bile leaks. It may be called a HIDA Scan or a gallbladder scan.
1. How is Scintigraphy (HIDA Scan) done?
A radioactive chemical is injected into the patient's vein. The chemicals are excreted by the liver into bile, then dispersed everywhere the bile goes – into the bile ducts, gallbladder, and intestines. A radio-sensing camera is placed on the patient's abdomen and an "image" of the liver, bile ducts, and gallbladder is obtained corresponding to where the radioactive chemical has traveled in the liver, sugar gall bladder, and gallbladder. Cholescintigraphy takes about two hours.
2. Scintigraphy in acute cholecystitis
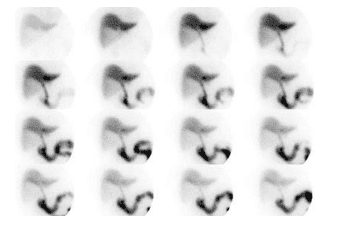
Biliary system imaging without gallbladder imaging after 4 hours is considered diagnostic of acute cholecystitis (Delayed imaging 1-4 hours in patients with normal liver function is a reliable marker of inflammation). chronic gallbladder).
Overall sensitivity and specificity of biliary scintigraphy for the diagnosis of acute cholecystitis are greater than 95% and 98%, respectively. In about 3.5% of cases of acute cholecystitis, the gallbladder is visualized in 1 to 4 hours - possibly secondary to incomplete cystic duct obstruction. The negative predictive value of a normal test (ie: gallbladder imaging within 1 hour) to rule out acute cholecystitis is greater than 99%.
No gallbladder imaging is a non-diagnostic finding when tracer is very poorly secreted or absent into the biliary tree, which can be seen in common duct obstruction or severe hepatocellular dysfunction (bilirubin). above 30 mg/dl).
Peri-gallbladder sign:
Refers to increased liver activity around the gallbladder without gallbladder imaging. The coronary sign appears as an active curved band along the hepatic margin above the gallbladder orifice and is often identified early on examination. It may be due to increased outflow and/or impaired radionuclide secretion by hepatocytes. Coronary sign is identified in approximately 20-30% of patients with acute cholecystitis, but it can also be seen in some patients with chronic cholecystitis. The positive predictive value for acute cholecystitis is about 95% when coronary signs are identified related to the absence of gallbladder visualization after one hour. Approximately 40% of patients with coronary signs will develop complicated cholecystitis (widespread necrosis, perforation, or lymphadenopathy of the gallbladder), so the presence of this finding suggests a more urgent need for surgery. Very rarely, gallbladder imaging is associated with coronary signs - this is still considered highly suspicious for acute or subacute cholecystitis.
Increased blood flow:
Increased blood flow to the gallbladder fossa region on radiographic angiography, increases the positive predictive value of not seeing the gallbladder for acute cholecystitis. Increased flow is seen in 88% of patients with cholecystitis; however, only 30% of patients with increased flow have cholecystitis.
Ductal cyst sign:
Dilated bile duct sign refers to an active nubbin that projects from the proximal end of the medial common bile duct to the fossa of the gallbladder. It is said to represent a patent cystic duct distal to the site of obstruction. This finding is observed in approximately 7% of patients with acute cholecystitis and should not be confused with a small, atrophic gallbladder. Ultrasound may be useful to demonstrate gallbladder size in these cases.
3. Differential diagnosis without showing gallbladder at one hour
Recent meal (patient must NPO at least 4-6 hours before examination) Fasting for more than 20 to 24 hours (The gallbladder is filled with bile. Sincalide can be given 30 to 60 minutes before the examination to empty the pouch). Hollow bile) Persistent Hyperpigmentation: Persistent hyperpigmentation during fasting leads to decreased bile production and cholestasis. There is no CCK-mediated gallbladder contraction due to lack of food entering the duodenum. This leads to bile stagnation and sludge formation due to water absorption. The radiometer could not get into the distended, sludge-filled gallbladder. Anterior cholecystectomy Acute pancreatitis Treat with CCK immediately before commencing examination (The gallbladder remains contractile and without tracer accumulation) Common/cystic duct obstruction: Cancer of the bile ducts of the bile ducts of the bile ducts. cystic duct or tumor compressing the cystic duct Severe hepatocellular dysfunction (Hepatitis, Cirrhosis): May lead to delayed or no discernible gallbladder. No gallbladder

4. False-positive test results for cholecystitis
An increased rate of false-positive tests is seen in patients with alternating severe illness, fasting, or hyperpigmentation (test specificity in these clinical settings is poor).
5. False-negative test for cholecystitis: (Normal study in patients with the disease)
In general, false-negative studies (gallbladder imaging in patients with acute cholecystitis) occur in less than 5% of patients and may be associated with:
Incomplete cystic duct obstruction Inflammation of the gallbladder Gallbladder accessory Diverticulum duodenum simulates gallbladder activity
6. Scintigraphy images in patients with chronic cholecystitis
The majority of patients with chronic cholecystitis have a normal gallbladder appearance (85-90%). Delayed gallbladder imaging (from 1 to 4 hours after examination) is considered fairly specific for chronic cholecystitis when seen, but delayed imaging may also be seen in a very small number of patients with inflammation. acute cholecystitis (3.5%). The longer the delay in visualization, the higher the correlation with chronic cholecystitis. Visualization of bowel activity before visualization of the gallbladder is an insensitive, but rather specific finding in patients with chronic cholecystitis (In most normal cases, the gallbladder is seen before bowel activity). This sign indicates chronic cholecystitis about 75% of the time.
Delayed bile-to-intestinal transit time (no bowel activity for one hour despite visualization of the gallbladder) has also been described in patients with chronic cholecystitis, and it has may be associated with associated pulpitis. Unfortunately, this finding can be seen in many other conditions including:
Normal (15%) Degraded common bile duct obstruction Chronic cholecystitis Sphincter of Oddi Dyskinesia Morphine is given before examination Sincalide for pre-examination: Due to the passage of bile into the recently emptied gallbladder. Total accessory gastric bypass S/P and vaginectomy Sepsis Small bowel obstruction
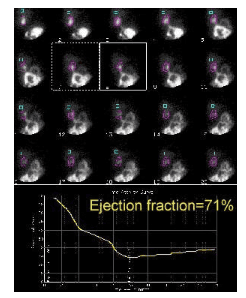
7. Gallbladder ejection fraction / Chronic non-stone cholecystitis
Chronic cholecystitis is relatively uncommon compared with chronic cholecystitis and accounts for 5-10% of cases of symptomatic chronic cholecystitis. The patient will often complain of right upper quadrant pain and biliary colic, but normal activities, including ultrasonography and hepatobiliary studies, are normal. Many of these patients were found to have chronic inflammatory changes in the gallbladder if they were to undergo surgery. Patients with chronically inflamed, partially obstructed, or dysfunctional gallbladder (gallbladder dyskinesia) will have an abnormal ejection response of the gallbladder to CCK. Abnormal ejection fraction of the gallbladder is considered to be less than 35% and is not affected by age.
Drugs and physiological drugs that can alter gallbladder contractility:
Morphine : Induces contractions of the sphincter of Oddi Atropine: Inhibits gallbladder emptying Calcium channel blockers: Reduces contractility by interfering into calcium-mediated smooth muscle contraction Diabetes: Neuropathy is associated with decreased contractility Vagal resection: Leads to decreased gallbladder contractility and increased gallbladder volume due to disruption of the cholinergic pathway paragraph. Achalasia- reduce ejection fraction by 50% Octreotide therapy Cholinergics: Enhance gallbladder emptying Hypercalcemia: Enhance contractility
8. Scanning image of non-stone cholecystitis
Acute cholecystitis accounts for only 2-5% of all cases of acute cholecystitis and it is often associated with surgery (postoperatively), major trauma, sepsis, hypersecretion, burns, urination diabetes, pancreatitis, or sickle cell disease. It may be due to a combination of stasis with increased bile viscosity and chemical irritation due to bile concentration, bacterial infection, and ischemia. Edema or noncalculous obstruction of the cystic duct may also play a role in its etiology. Cystic duct obstruction can sometimes be incomplete, allowing some tracer to enter the gallbladder and lead to false-negative test results. Sincalide infusion will usually show little or no gallbladder contraction, but this finding may also represent chronic cholecystitis. A labeled white blood cell test may be necessary to confirm the diagnosis. Cholescintigraphy has a sensitivity of 60 to 92.5% for acute cholecystitis Ultrasonographic findings in acute cholecystitis include moderate echogenicity (pus) in the gallbladder lumen.
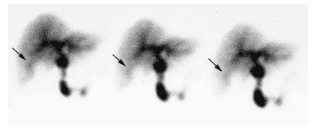
9. Scanning image of biliary obstruction
Ultrasonography has low sensitivity in detecting common ductal stones (11 to 30%) and may not show intrahepatic catheter dilation. Obstruction of the extrahepatic bile duct causes an increase in hydrostatic pressure in the bile duct until no longer is the ability to excrete hepatocytes. In acute common bile duct obstruction (0 to 24 hours) there is usually a rapid liver uptake of the tracer with no biliary tree appearance and no digestive activity (unless the obstruction is partial). Liver function remains normal during this early period. Between 24 and 96 hours, liver function declines slightly to moderate. After 96 h, liver absorption is very poor and scintigraphic findings are difficult to distinguish from hepatitis.
If the biliary tree is seen, the tracer activity in the normal common bile duct will be less on the 2-hour image, compared with the 1.5-hour image. If the activity of the common bile duct is unchanged or sharply increased on subsequent images, some degree of obstruction is likely. Intrahepatic cholestasis may produce a pattern resembling complete common bile duct obstruction.
10. Causes of radiographs that are absorbed in the liver but not excreted
Acute common bile duct obstruction: Gallstone disease Acute pancreatitis Carcinoma: ( Cholangiocarcinoma, ductal carcinoma or carcinoma of the head of the pancreas) More commonly, tumors produce the Gradual obstruction with hepatocellular dysfunction and slow accumulation of scintigraphy in the liver. Infection: Progressive cholangitis cannot be ruled out when intestinal motility is delayed or cannot be visualized Cholestasis: More common is hepatic malabsorption (slow blood clearance) with slow biliary excretion related to cholestasis. Causes of cholestasis include gram-negative sepsis and drugs. Agents such as chlorpromazine (Dilantin) and oral contraceptives are often associated with decreased liver function and delayed tracer accumulation.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.