This is an automatically translated article.
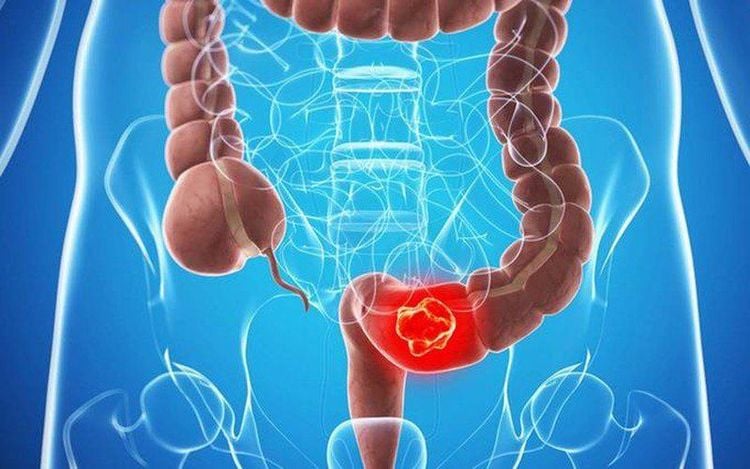
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Colorectal cancer (CRC) is the third most diagnosed and the second highest cause of death worldwide. The application of colorectal cancer screening has improved morbidity and mortality. However, as the coronavirus disease 2019 (COVID-19) pandemic began, healthcare resources were dwindling away from colorectal cancer screening services, leaving the number of patients waiting for screening tests to continue. backlog filter.
This can have a significant effect on colorectal cancer mortality, as delayed screening can lead to late-stage cancer at diagnosis. Strategies to overcome COVID-19-related disruption include using stool-based cancer testing, developing screening protocols based on individual risk factors, expanding telehealth and increased access to open endoscopy.
1. Frequency of colorectal cancer
Colorectal cancer (CRC), which includes colon and rectal cancer, is the third most diagnosed cancer globally. It comprises more than 10% of all cancer diagnoses, with an estimated 1.9 million colorectal cancer diagnoses by 2020. In terms of mortality, colorectal cancer ranks second among the numbers. cancer is the leading cause of death worldwide. It causes more than 900000 deaths annually, often due to diagnosis in advanced clinical stages.
Specifically, in the United States, there are 147950 colorectal cancer diagnoses expected for 2020, with 53200 colorectal cancer deaths. Studies show that the significant regional variation in incidence is due to differences in behavior and lifestyle as well as disparities in access to colorectal cancer screening. Racial and socioeconomic disparities in colorectal cancer also exist, with the highest morbidity and mortality among non-Hispanic blacks and American Indians/Alaska Natives. (AI/ANs), especially colorectal cancer is more likely to be diagnosed in people with low socioeconomic status.
2. Economic burden of colorectal cancer
In terms of economic burden, Medicare Program Surveillance, Epidemiology, and End Results data for 2007-2012 show an average spending of $6,3063 per patient on colorectal cancer. colon. The more advanced stage at diagnosis is associated with higher annual spending. The advent of good colorectal cancer screening is a major driver of higher survival. Attempts at early detection and removal of polyps allow the diagnosis of previously unknown disease. This early diagnosis and resection of precancerous or non-metastatic polyps have reduced mortality in the long term.
In the United States, End of Year Outcomes, Epidemiology, and Surveillance Program data from 1991 to 2011 show a 35% reduction in morbidity with a 37% reduction in mortality associated with screening programs. . A cost-effectiveness study found that if screening rates were increased to 80%, more than three times more colorectal cancer deaths could be avoided at a third of current costs. .
3. The situation of coronavirus disease 2019 (COVID-19) in the world
Coronavirus disease 2019 (COVID-19) started in late 2019, March 30, 2020, it has spread to 203 countries and has officially declared a global pandemic. As of May 1, 2021, there are a total of 84474195 confirmed cases, with 1848704 deaths globally. 222 different countries, regions or territories are affected with cases.
The initial impacts of COVID-19 were severe due to both the contagion and lack of proper preparation and anticipation. In the United States, there has been rapid mobilization and distribution of existing health care resources and social distancing efforts. The trend in many affected countries, such as Italy, France, the United Kingdom, Germany and Spain, is an initial outbreak in March 2020, followed by a decrease in the number of cases after May. 2020. Then a new outbreak of COVID-19 around November 2020, resulting in a “second wave”.
4. General recommendations by country
The COVID-19 pandemic has continued since March 2020 and the consequences must be considered. During this time, patients are advised to avoid unnecessary hospital and emergency department visits. Non-urgent visits as well as elective procedures and surgeries have been canceled during the outbreak. Changes in health care use during this time could lead to serious long-term effects.
Specifically, new challenges have arisen related to cancer prevention and treatment, as surgeries and cancer screenings are cancelled, treatment plans are disrupted. This raises many barriers to colorectal cancer screening, which should be addressed quickly.
5. Barriers to colorectal cancer screening due to Covid-19
COVID-19 has caused a major disruption in healthcare usage, as patients are encouraged to avoid hospitals and reschedule occasional visits and elective procedures . To conserve healthcare resources and direct them toward efforts to combat COVID-19, cancer screening services for patients have been halted.
As of March 12, 2020, the American Cancer Society recommends deferring cancer screening plans. Endoscopic units are recommended to prioritize necessary procedures and specifically consider postponing non-urgent procedures. This dramatic reduction in endoscopic procedures greatly affects the volume of colorectal cancer screening and may have a lasting impact on these diagnoses. In the United States, from January 20, 2020 to April 21, 2020, colorectal cancer screening rates are estimated to have fallen by 85%. As of June 16, 2020, the rate is still 36% lower than previous COVID-19 levels.
6. Decline in endoscopic procedures is also reflected
A cross-sectional study analyzing health insurance claims for patients across the US found that clinic visits decreased by 68% when compared from April 2020 to April 2019. In this year, the number of telemedicine visits increased by 40.81%. Although the relative increase in telemedicine was significant, the absolute increase did not offset the decrease in clinic visits.
This may indicate that patients with nonspecific cancer symptoms such as fatigue, weight loss, or changes in bowel habits do not choose to speak to their doctor. People presenting via video or phone consultations may have missed diagnoses due to lack of physical examination and doctors' inability to use their intuition.
Patients may also feel more embarrassed and uncomfortable when expressing concerns about alarming symptoms in the form of telemedicine. When patients develop symptoms of cancer that are detected during their examination, management may still be delayed. If only emergency colonoscopy is performed, patients with symptoms suggestive of colorectal cancer will prolong the time of diagnosis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Kadakuntla A, Wang T, Medgyesy K, Rrapi E, Litynski J, Adynski G, Tadros M. Colorectal cancer screening in the COVID-19 era. World J Gastrointest Oncol 2021; 13(4): 238-251 [PMID: 33889276 DOI: 10.4251/wjgo.v13.i4.238]