This is an automatically translated article.
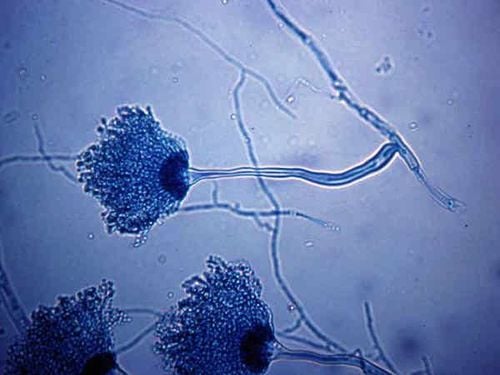
Aspergillus is a fungus that can lead to a variety of infectious diseases, depending on the host immune status or lung structure. In particular, Aspergillus lung disease is an invasive form that occurs mainly in severely immunocompromised patients, which if not treated promptly will affect the patient's life.
1. What is Aspergillus lung disease?
Aspergillus lung disease is a severe pneumonia caused by the fungus Aspergillus (usually Aspergillus fumigatus). Different species of Aspergillus are always present everywhere in the surrounding environment, are considered benign if there is exposure to the lungs with normal structure and the body's immunity is healthy. If either of these is abnormal, it is possible that this benign fungus may be causing the disease. Therefore, the disease can be seen in severely immunocompromised patients and those with chronic obstructive pulmonary disease.
On the other hand, Aspergillus is a fungus that can reside in pre-existing lung cavities, especially those left by pulmonary tuberculosis. In this environment, the fungus grows and, because it moves freely in the cavity, is often spherical in shape and is called aspergilloma.
Chronic necrotizing aspergillosis can be locally invasive, with the lung being a typical target organ with pneumonia. In particular, Aspergillus in the lungs is mainly seen in patients with immunodeficiency.
2. Risk factors for Aspergillus lung infection
Alveolar macrophages are the first line of defense against inhaled Aspergillus fungal spores. Accordingly, the main risk factor for Aspergillus lung disease is immunosuppression, including neutropenia, organ transplantation, long-term treatment with high-dose corticosteroids, hematologic malignancies, and toxic therapy. cytology, advanced AIDS, and chronic granulomatous disease.
Of these, the most important risk factor is leukopenia, especially when the absolute neutrophil count is <500 cells/mm of blood. The risk of Aspergillus lung disease is strongly correlated with the duration and severity of leukopenia.
In addition, patients with chronic obstructive pulmonary disease require prolonged parenteral nutrition, multiple antibiotics, and long hospital stays, as well as the need for intensive care (ICU). increases the risk of fungal infections, including Aspergillus.
Bệnh phổi do nấm Aspergillus là một viêm phổi nặng
3. What are the clinical manifestations of Aspergillus lung disease?
In most cases, Aspergillus enters the lower respiratory tract by inhaling infectious spores. In addition, less commonly, Aspergillus lung disease can also start in sites other than the lungs, such as the sinuses, gastrointestinal tract, or skin (through an intravenous catheter, prolonged skin contact with bandages). stick or burn).
Symptoms of Aspergillus lung disease are often nonspecific and resemble bronchopneumonia. Symptoms include:
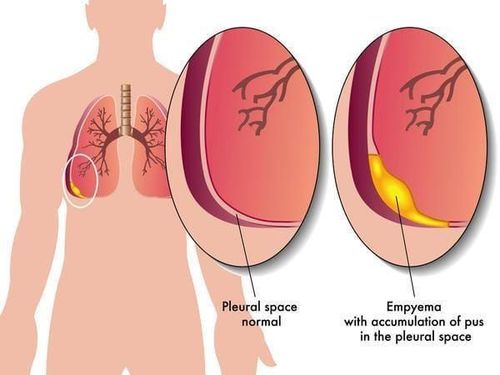
Fever not responding to antibiotics. Cough, phlegm and difficulty breathing. Patients may also present with pleuritic chest pain (due to vascular invasion leading to thrombosis causing a small pulmonary infarction) and hemoptysis, which is usually mild, but can be severe. Aspergillus infection can also spread by blood to other organs, including the brain. This can lead to seizures, sphincter dysregulation, cerebral infarction, intracerebral hemorrhage, meningitis, and epidural abscess.
4. Diagnostic criteria for lung Aspergillus infection
The diagnosis of Aspergillus lung disease in general remains challenging. In particular, early diagnosis of pulmonary Aspergillus infection in severely immunocompromised patients is very difficult, and patients with risk factors for invasive disease should be suspected.
The gold standard in the diagnosis of Aspergillus lung disease is histopathological examination of the lung parenchyma by thoracoscopy or open lung biopsy for the presence of acute, branching, septal mycelium enter lung tissue with Aspergillus-positive culture from one site. In parallel, histopathological examination also allows the exclusion of other diagnoses, such as malignancy or non-fungal infectious disease.
Besides, the isolation of Aspergillus in sputum samples also has diagnostic significance, although it depends heavily on the immune status of the host. In immunocompetent patients, fungal infections are almost non-clinical.
Chest radiographs are rarely used in the early stages of the disease because of the high rate of nonspecific changes. The usual findings of Aspergillus lung disease are round, pleural infiltrates, sometimes suggestive of pulmonary infarction and foci of necrosis. Pleural effusion is an uncommon feature. Chest computed tomography (CT), especially when combined with high-resolution images, is much more useful than conventional radiographs. Therefore, this tool, when performed routinely, will help diagnose earlier and improve patient outcomes.
Bronchoscopy with bronchoalveolar lavage is an invasive diagnostic tool that is often useful in diagnosing Aspergillus infections of the lungs, especially in patients with diffuse pulmonary involvement. In addition to sampling for staining and fungal culture, intervention may be useful in detecting Aspergillus antigens in bronchial fluid as well as excluding other infections. Transbronchial biopsy may be considered in some suspected patients.
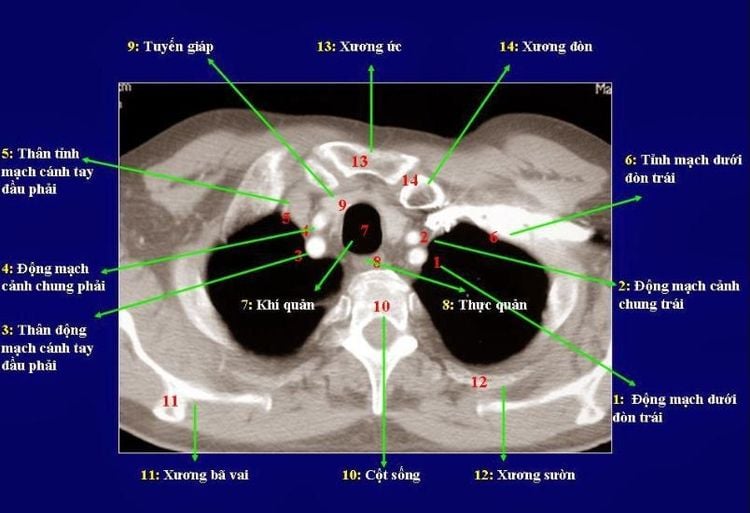
Chụp cắt lớp vi tính lồng ngực sẽ giúp chẩn đoán sớm nhiễm nấm Aspergillus ở phổi.
5. How to treat Aspergillus lung disease?
Despite the introduction of several new antifungal drugs, the treatment of lung disease caused by Aspergillus is still difficult and the mortality rate is high. Accordingly, therapy should be considered as soon as there is clinical suspicion of Aspergillus lung disease.
Amphotericin B has been the first-line component of Aspergillus lung disease for many years, with a recommended dose of 1–1.5 mg/kg/day. However, this drug can cause serious side effects, including nephrotoxicity, electrolyte disturbances, and hypersensitivity. To reduce these side effects, newer lipid-based preparations of amphotericin B (such as amphotericin B and lipid-complex amphotericin B) have been introduced, but higher doses are required for comparable antifungal efficacy.
A new broad-spectrum triazole, voriconazole, has been approved for the other initial treatment of invasive aspergillosis. Currently voriconazole is considered the treatment of choice in many patients with Aspergillus infections. Voriconazole is available in both intravenous and oral forms. The recommended dose is 6 mg/kg twice daily intravenously on the first day, followed by 4 mg/kg/day. After 7 days, a switch to 200mg orally twice daily may be considered. Voriconazole has milder side effects and is much better tolerated than amphotericin B. The most common adverse event was visual disturbances, described as blurred vision, photophobia and altered color perception. Abnormalities in liver function tests and skin reactions are less common side effects. However, voriconazole has been associated with a number of significant drug interactions, such as with cyclosporine, warfarin, terfenadine, carbamazepine, quinidine, rifampin, statins, and sulfonylureas. In addition, another broad-spectrum triazole, posaconazole, is effective and safe as salvage therapy in patients with Aspergillus infections resistant to standard antifungal therapy.
Echinocandin derivatives such as caspofungin, micafungin and anidulafungin are also effective agents in the treatment of Aspergillus pulmonary disease resistant to standard therapy or if patients cannot tolerate first-line agents. While polyenes and azoles target fungal cell membranes, echinocandin inhibits the β-d-glucan component of the fungal cell wall. Therefore, a combination antifungal therapy may be a strategy for the treatment of resistant Aspergillus lung disease.
The duration of treatment for Aspergillus lung disease should depend on the clinical and radiological response of the patient. In most cases, treatment lasts from a few months to more than a year. Prerequisites for treatment discontinuation included clinical and radiographic improvement, microbiological clearance, and reversal of immunosuppression. Reversal therapy in responding patients should be considered if immunosuppression continues or if the patient requires additional cytotoxic and other antifungal therapy.
In terms of surgical intervention, pneumonectomy generally has a limited role but will become important in cases of pulmonary Aspergillus invasion of bone, burn wounds, epidural abscesses, and epidemic diseases. glasses. Intervention should also be considered in cases of massive hemoptysis, pulmonary involvement near major vessels and the pericardium, or residual focal lung damage in patients who are continuing to be immunosuppressed, as well as those with who are expected to receive immunosuppressive therapy in the future.
Immunomodulatory therapy may be indicated to reduce immunosuppressive levels and as an adjunct to antifungal therapy for pulmonary A spergillus. Components of the therapy include intrinsic stimulating factors, such as granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF), interferon-γ, thereby indirectly increasing the phagocytic activity of neutrophils against fungi, including Aspergillus.
Finally, granulocyte infusion is another potential adjuvant therapy, especially for patients with persistent neutropenia and life-threatening infections that cannot be treated with conventional therapy.
In a nutshell, Aspergillus lung disease is a general term used to describe pneumonia caused by infection with a fungus of the Aspergillus species. Immunodeficiency is a risk factor for Aspergillus infection in the lungs. Because the symptoms are not clear in high-risk subjects, it is necessary to screen for Aspergillus fungus in the lungs for early detection and aggressive treatment from the beginning to minimize the risk of drug resistance later on.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.