This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Nguyen Xuan Tinh - Anesthesiologist - Resuscitation - Department of General Surgery - Vinmec Phu Quoc International General Hospital. Doctor Nguyen Xuan Tinh has more than 18 years of experience studying and working in the field of Anesthesia - Resuscitation.In order to treat non-invasive or recurrent bladder cancer, patients need cystectomy. Cystectomy also helps to treat other pelvic tumors such as prostate, endometriosis, ... Anesthesia in optic surgery to anesthetize, reduce surgical pain.
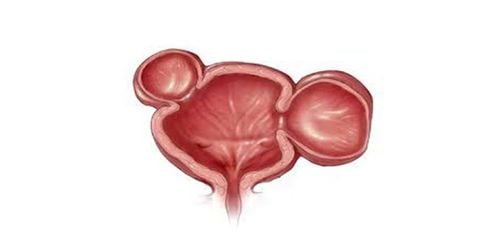
1. Cystectomy
Cystectomy is the surgical removal of the bladder. In men, a radical cystectomy requires removal of the prostate gland and seminal vesicles. In women, the uterus, ovaries, and part of the vagina will need to be removed.After surgery, the patient will change the urinary tract. Usually, the patient will have a stoma created to store and remove urine from the body. The patient needs to urinate every few hours during the day or as initially recommended by the doctor.
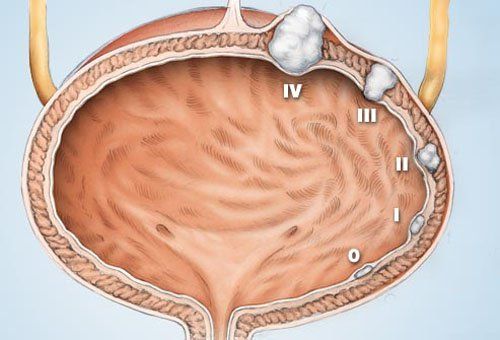
Patients may be prescribed cystectomy by the doctor in case a tumor is detected in the bladder or metastases from the bladder are developed. In addition, under the following cases, the patient will be performed cystectomy.
Birth defects affecting the urinary system Nervous or inflammatory disorders affecting the urinary system
2. Anesthesia in cystectomy
Anesthesia in cystectomy is intended to satisfy the need for anesthesia and analgesia, by local anesthesia administered with local anesthetic into the subarachnoid or epidural space.Anesthesia in cystectomy will not be performed in case the patient and the patient's family refuse. Because the anesthetic process requires the use of local anesthetic, it is contraindicated when the patient is allergic to local anesthetic. In addition, the cases of inflammation of the needle puncture site, lack of adequate circulating volume, shock, coagulopathy, insufficient time stopping anticoagulation, constricted mitral stenosis, aortic valve constriction, severe decompensated heart failure ... will be contraindicated in anesthesia in cystectomy.
3. Anesthesia procedure in cystectomy
3.1. Prepare
On the hospital side: To perform anesthesia in cystectomy, the surgical team needs doctors and nurses specializing in anesthesiology and resuscitation. At the same time, the means and tools need to be fully prepared. Specifically:Resuscitation facilities: oxygen source, Ambu balloon, mask, intubation equipment, anesthesia machine with breathing, electric shock machine, suction machine... Resuscitation medicine: fluids, medicine: ephedrine, adrenaline... Anticonvulsants: barbituric family, benzodiazepines, muscle relaxants, intralipid 10-20%... Routine monitoring means: electrocardiogram, blood pressure, oxygen saturation, breathing rate... Pump needles of all sizes, gloves, sterile gauze, pince, antiseptic alcohol, sterile gauze, needles for spinal anesthesia of all sizes... Local anesthetics: bupivacaine, levobupivacaine, ropivacaine... can be combined with drugs morphine family (morphine from 100-300 mcg; fentanyl 25-50 mcg, sulfentanil 2.5-5 mcg...). Dosage is based on weight, height and body condition of the patient: bupivacaine dose from 3-12mg; levobupivacaine from 5-12mg; ropivacaine dose from 5-20mg; Reduce dose for people > 60 years old, anemia, pregnancy. On the side of the patient: In addition to the patient needing to be examined and explained to the patient before the operation, you need to inform the doctor about the drugs you are taking as well as the habit of using caffeine. or wine.
If the patient has a habit of smoking, quit smoking before deciding to have surgery. Patients are instructed to clean the anesthetic area to avoid infection. In case, the patient is agitated, the doctor may prescribe a sedative from the day before surgery. At the same time, the patient's medical record according to the regulations of the Ministry of Health.
3.2. Procedure
The person performing the operation should wear a hat, mask, wash hands, wear a shirt, and wear sterile gloves. First, disinfect the needle puncture area 3 times. The patient will receive spinal anesthesia in a sitting or lying position. If in the lying position, have the patient lie on their side with their back bent, knees pressed against the abdomen, chin pressed to the chest. If in a sitting position, the patient sits with his back arched, head bowed, chin resting on his chest, legs stretched out on the operating table or feet on the chair.Prophylaxis of hypotension: Place an intravenous line for the patient to effectively prevent hypotension and give fluids from 5-10 ml/kg (for adults).
Step 1: Spinal anesthesia technique
When administering spinal anesthesia, the doctor will perform in the midline (puncture between the 2 vertebrae, position L2-L3 to L4-L5) or lateral line (interstitial puncture) midline 1-2cm, direct needle to midline, up, forward). Aim the bevel of the anesthetic needle parallel to the patient's spine and insert the needle until a sensation of loss of resistance is achieved as the needle passes through the dura. Finally, to check for CSF effusion, turn the bevel of the needle toward the patient's head and inject the anesthetic. Step 2: Epidural technique
The epidural technique will numb the area with 1-2% lidocaine. At the same time, the doctor will perform the midline (puncture between the 2 vertebrae, position L1-L2 to L3-L4) or lateral line (punch 1-2cm from the midline, direct the needle into the midline, up). , out first). Assess for correct needle position by loss of resistance and absence of regurgitation of cerebrospinal fluid and blood. The next step is to turn the needle bevel face up, slowly insert the catheter with a length of 3-6cm in the epidural space and withdraw the needle Tuohy The drugs used are: lidocaine 2% 10-20ml; bupivacaine 0.25-0.5% 10-20ml; ropivacaine 0.25-0.5% 10-20ml; levobupivacaine 0.25-0.5% 10-20ml. Combination drugs: morphine 30-50mcg/kg; sufentanil 0.2mcg/kg should not exceed 30mcg/kg; fentanyl 25-100mcg. Continuous infusion: bupivacaine 0.125-0.25%, running rate 4-6ml/hour; ropivacaine 0.125-0.25% 4-10ml/hour; levobupivacaine 0.125-0.25% 4-10ml/hour. Concentrations of combination drugs: morphine 10-20mcg/ml; fentanyl 1-2mcg/ml; sufentanil 0.5 mcg/ml.

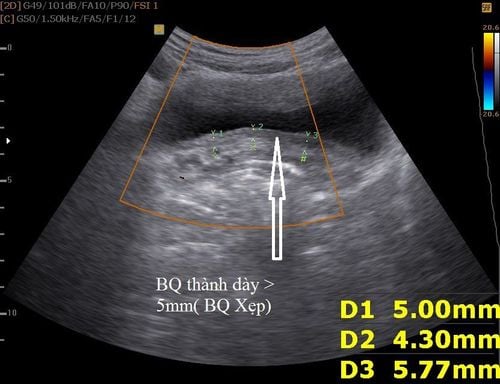
4. Follow up
Vital signs: consciousness, heart rate, electrocardiogram, arterial blood pressure, capillary oxygen saturation. Degree of sensory and motor blockade Undesirable effects of spinal anesthesia. Criteria for transferring patients from the recovery room: no hemodynamic and respiratory disorders; full recovery of movement, sensory block below T12 (below the inguinal fold).5. Possible complications of anesthesia in cystectomy and how to manage
Patients need to stay in the hospital for 5-6 days after surgery to recover to absorb fluids and nutrients. Gentle walking will promote bowel function recovery, improve circulation, help prevent stiffness and blood clotting.However, like any medical treatment, patients with anesthesia during cystectomy may experience some unwanted complications. Here are some of the possible complications equivalent management options:
Since cystectomy is a surgery not only to remove the bladder but also to create another urinary tract, it will stretch according to the additional risks such as: dehydration, electrolyte abnormalities, urinary tract infections, intestinal obstruction, ureteral obstruction. use anti-anaphylaxis regimen according to the Ministry of Health. It is necessary to stop using local anesthetics, anticonvulsants, respiratory and circulatory resuscitation, intralipid infusion when poisoning with local anesthetics bupivacaine and ropivacaine when the patient has signs Signs of local anesthetic toxicity Low blood pressure and slow pulse should be treated with vasopressors and fluid resuscitation. Headache: lying motionless, giving enough fluids, using pain relievers, patching the dura with autologous blood (Blood Patch). Use antiemetics when the patient feels nauseous and vomiting, and always control blood pressure Urinary retention: warm compresses, bladder catheterization if necessary. General spinal anesthesia: emergency respiratory and circulatory resuscitation. Other complications: hematoma around the spinal cord, spinal cord injury, cauda equina syndrome, meningoencephalitis. Further consultation and investigation is required to identify the lesion. Failure of anesthesia requires switching to anesthesia. With the goal of bringing patients the most advanced medical techniques in the world, minimizing complications and risks, Vinmec International General Hospital has applied the ESP technique. This is an analgesia technique that can completely replace analgesia morphine in open heart surgery and thoracic surgery in both adults and children with many outstanding advantages:
Helps to relieve pain comprehensively, without complications, shorten the time of active resuscitation, eliminate the risk of postoperative pain and chronic pain in 96% of heart surgery patients. No direct effect on spinal cord and anatomical structures of nerves Safer due to ultrasound guidance There were no cases of needing to add morphine analgesia when skin incision, sternum saw. Significantly reduce the dose of painkiller Sufentanil during surgery. Pain level after extubation, exercise, and extubation (VAS <3). There were no complications of hematoma, hypotension or excessive anesthesia, respiratory depression, anesthetic toxicity.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.