This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Not only directly affects the lungs, corona virus also affects other internal organs in the patient's body, including the liver. So how is the reliable physiological mechanism of Covid-19 causing liver cell damage and liver disease to be understood?
SARS-CoV-2 can cause liver damage in a number of ways including direct cytotoxic effects of the virus on ciliary/hepatocytes, immune-mediated injury, hypoxia, and infection. blood. Indeed, the immediate cytotoxic effect of SARS-CoV-2 through its potential pseudotarget, the angiotensin-converting enzyme-2 receptor, is highly expressed in hepatocytes and bile cells, causing The liver as an organ in addition to respiration, increases susceptibility to pathological findings. However, the underlying pathogenesis of liver disease associated with COVID-19 with abnormal liver function tests (LFTs) is still not fully understood. The authors therefore contrasted COVID-19-associated liver injuries with increases in LFTs in the association between pre-existing liver diseases and COVID-19, and identified a triad of associated pathophysiologies. of COVID-19, hepatocellular damage, and liver disease. This review summarizes recent findings on the aggravating role of COVID-19 in pre-existing liver disease and vice versa, as well as international guidelines for patient care, management, and treatment recommendations. COVID-19 has liver disease.
1. Reliable physiological mechanism of Covid-19 causing liver cell damage and liver disease
Epidemiological studies have characterized hepatic dysfunction and the effect of SARS-CoV-2 infection on hepatocytes in COVID-19 patients by elevated levels of liver injury markers such as ALT, AST and bilirubin. It has been previously stated that the SARS-CoV and MERS-CoV viruses mainly affect the upper respiratory tract but also the liver. Despite the immediate and direct action of SARS-CoV-2 via latent targets on epithelial cells of the pulmonary alveoli as well as the respiratory tract, emerging evidence suggests that high expression of ACE2 receptors in the liver make it susceptible to SARS-CoV-2 infection. Pathological examination of COVID-19 patients confirmed cellular damage in the lungs and recently confirmed SARS-CoV-2 infection as the etiology of liver disease. Proposed mechanisms implicated in COVID-19 liver injury include hepatic deformity directly related to viral insult, cytokine storm-related liver injury, and deficiency-related ischemia oxygen caused by COVID-19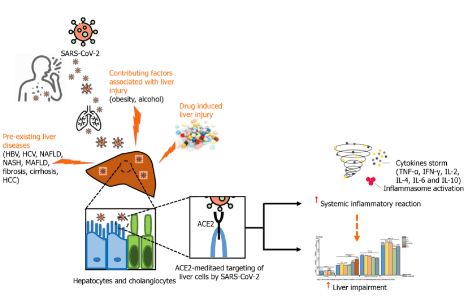
2. Pathogenesis of acute respiratory syndrome-coronavirus type 2 and hepatic immune response
ACE2: Transfer enzyme 2; HBV: Hepatitis B virus; HCC: Hepatocellular carcinoma; HCV: Hepatitis C virus; IFN: Interferon; IL: Interleukin; MAFLD: Metabolic-associated fatty liver disease; NAFLD: Non-alcoholic fatty liver disease; NASH: Non-alcoholic steatohepatitis; SARS-CoV-2: Severe acute respiratory syndrome-coronavirus type 2; TNF: Tumor necrosis factor. Liver failure due to COVID-19 may directly correlate with hepatocyte infection with SARS-CoV-2. Approximately 2%-10% of COVID-19 patients with diarrhea have confirmed SARS-CoV-2 RNA in stool and blood samples, which implies possible exposure to the virus in the liver. The affinity of SARS-CoV-2 and SARS-CoV for the ACE2 receptor indicates the respective target sites, mainly the upper respiratory tract, lung tissue, and liver bile cells, where the virus replicates and expresses symptoms associated with COVID-19. Against this background, Zhao et al studied a model of SARS-CoV-2 infection in human liver tubule cells. They reported genomic evidence that infection with the SARS-CoV-2 virus leads to dysregulation of the bile-cell barrier and bile acid transport function. The study suggests that altered bile cell functions may be the result of a direct cytotoxic effect of SARS-CoV-2 on target cells expressing ACE2 and TMPRSS2. Cytokine storm is one of the hallmarks of infectious and non-infectious diseases capable of causing severe multi-organ damage
Establishment of a cytokine environment is a multifactorial network involved in response immune response to invading antigens with the interaction of activated host immune and inflammatory cells. Consistent with the concept of a cytokine storm in COVID-19 patients, Han et al. [65] performed a prospective cohort study at a local hospital in Wuhan, China that enrolled 102 patients. confirmed COVID-19 and 45 healthy control volunteers. They analyzed serum profiles of inflammatory cytokines, including tumor necrosis factor-, interferon-, interleukin (IL)-2, IL-4, IL-6, IL-10, and C-reactive protein. (CRP) by immunoassay. Significantly increased levels of inflammatory markers and CRP were seen in COVID-19 patients compared with healthy volunteers. Furthermore, IL-6 and IL-10 levels were significantly higher in critically ill patients than in moderate or severe COVID-19 patients, suggesting that increased IL-6 and IL-10 may allow rapid diagnosis of patients at increased risk of fatal disease. Furthermore, Wang et al reported conspicuous cellular disease associated with COVID-19. The severity of SARS-CoV-2 infection is associated with disturbed liver enzyme levels, increased alveolar oxygen gradient and GGT levels, decreased albumin and CD4+ T cells and circulating B lymphocytes. The main histological features of COVID-19 liver infection are programmed cell death and dual hepatocytes.
Liver dysfunction in severe COVID-19 is accompanied by abnormal activation of the coagulation and fibrinolytic pathways. Liver dysfunction in severe COVID-19 accompanied by abnormal activation of the coagulation and fibrinolytic pathways, moderately decreased platelet count, increased neutrophil count and white blood cell ratio neutrophils on lymphocytes, and high ferritin levels. Such laboratory findings are considered nonspecific markers of inflammation, but altered levels may coincide with failure of innate immune regulation during severe COVID-19 progression. . Indeed, altering immune homeostasis triggers coagulation and NETosis, and subsequently affects systemic iron metabolism secondary to macrophage activation
3. Recommendations for the management of covid-19 patients with pre-existing liver diseases
WHO has approved comprehensive guidelines to enhance care and management of COVID-19 patients and provides up-to-date guidance for physicians and clinicians. That report addresses best practices for the management of severe acute respiratory infections (SARI), including infection prevention and control measures and supportive care for COVID-19 patients. Furthermore, key considerations focus on the recognition and treatment of patients with SARI through appropriate diagnosis, early supportive treatment, management of acute respiratory failure and septic shock, prevention of complications, and the use of specific COVID-19 treatments.
Indeed, patients with chronic liver disease do not appear to be over-represented in the cohort of patients with COVID-19, where they represent less than 1% of reported cases. These observations suggest that patients with chronic liver disease may have a reduced risk of severe SARS-CoV-2. However, the risk of infection and/or the risk of a severe episode of COVID-19 may vary depending on the nature of the chronic liver disease and the presence or absence of fibrosis or advanced cirrhosis. Against this backdrop, the European Association for the Study of the Liver, the European Society of Clinical Microbiology and Infectious Diseases, and AASLD have provided comprehensive guidance for physicians and clinicians on the care of patients. patients with chronic liver disease in the early stages of the COVID-19 pandemic.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














