This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer and treatment results are often unsatisfactory. The high recurrence rate after monotherapy suggests the need for a combination of modalities, including radiotherapy (RT).
International guidelines from North America, Europe and Asia make treatment recommendations based on different classification systems. However, not all of these guidelines cover radiation therapy and the role of combined modalities. Therefore, this study reviewed the clinical evidence for different combined modalities in the management of HCC, focusing on the role of radiotherapy and in particular modern advanced radiotherapy techniques and interaction with game-changing immunotherapy.
1. The role of radiotherapy in HCC
Has been used as a salvage or palliative treatment in the past and only a few guidelines address the role of radiotherapy. However, in the modern era, radiation therapy is indicated at all stages (ie, very early to late stages of HCC). Notably, radiation therapy can be used as a single therapy or as an essential component of a combined regimen. Current treatment recommendations based on BCLC stage and potential role of radiation therapy are summarized in the table below.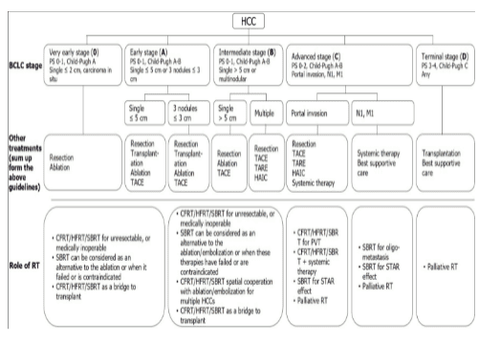
2. Different radiotherapy techniques
Photon therapy:
The most commonly available beam therapy of radiation therapy is photons. In the management of HCC patients, several photon beam delivery systems of external beam radiation therapy (EBRT) are clinically available, such as conventional fractionated radiation therapy (CFRT), radiotherapy segment reduction (HFRT) and SBRT. CFRT is usually delivered daily from 1.8 to 2 Gy, and HFRT is characterized by a large daily dose (ie, > 2 Gy) under precise radiotherapy conditions. Clinically, HFRT is a useful strategy to improve dose intensity and subsequently tumor control. Both CFRT and HFRT can be delivered using three-dimensional spherical radiation therapy (3DCRT), intensity modulated radiation therapy (IMRT), and Volume Modulated Arc Therapy (VMAT). The role of stereotactic whole-body radiotherapy Notably, SBRT (Study Whole Body Radiation Therapy), also known as SABR, is an advanced technique of EBRT that delivers very high doses of radiation in a very precise manner. a limited number of treatment segments (ie., usually 3-6 parts and >5 Gy each) in a 1-2 week course of treatment. For more focused and accurate delivery of SBRT, advances across the entire spectrum of radiotherapy are needed, including imaging, immobilization, targeting, treatment planning, and imaging guidance on aircraft and respiratory motion management (RMM). Only advanced IMRT or VMAT with or without a non-coplanar beam design can be used for SBRT delivery. These advances lead to better dose delivery, delivering higher doses within the tumor, and producing doses that quickly fall off-target. Therefore, SBRT may improve tumor control and reduce radiation dose to surrounding normal tissue, to reduce radiation toxicity. Because of this dual benefit of enhancing treatment effectiveness, For patients who cannot be successfully treated with SBRT, CFRT combines with two or more advanced irradiation techniques, such as combined VMAT and Booster. Simultaneous integrated internal displacement enhancement (SIEB), may be useful for achieving better therapeutic efficacy (i.e., better tumor control with minimal radiation toxicity) than conventional CFRT, including even for elderly HCC patients with inoperable disease Proton therapy:
Charged particle radiations, including proton beam therapy (PBT) and carbon-ion radiation therapy, have dosimetric features unique quantity. That is, they remove the low-dose bath volume far from the target region that is associated with the photons. This rejection is due to the characteristic Bragg peak of charge carriers that accumulate irradiation energy mainly in the targeted tumor area and result in a dose close to zero beyond the end of its path. Therefore, charged particle irradiation is an excellent option to improve normal liver and minimize side effects such as radiation-induced liver disease (RILD). It is also possible to increase the dose to cure unresectable giant HCC. Park et al. reported that increasing the dose may enhance HCC tumor control. Kim et al further confirmed that increasing the proton dose is safe and effective; They suggested that EQD2 ≥ 78 Gy-equivalent (GyE) could be distributed to achieve reasonable tumor control. According to tumor location, the University of Tsukuba proton research group developed different PBT dosing procedures. Extending the concept of SBRT “No Fly Zone” lung cancer, peripheral liver tumors located >2 cm from the portal or gastrointestinal (GI) region can be treated with reduced fractionation 66 GyE protons in 10 small portions. On the other hand, for tumors located within 2 cm adjacent to the hepatic peduncle region, a small dose per portion with 72.6 GyE in 22 fractions should be considered. For tumors located 2 cm from the GI tract, 77.0 GyE can be given in 35 subsections Several studies report the use of PBT for focal HCC with excellent local control, ranging from 80 % to 100%, even for very large unresectable HCCs, due to increased dose and decreased liver function. Furthermore, Sanford et al. reported that the overall survival (OS) benefit of proton-radiation versus photon-radiation could be attributed to the reduced incidence of RILD. Hsieh et al further identified predictors of RILD in PBT-treated HCC patients beyond the conventional notion of minimizing mean hepatic dose. A "volume-response" relationship between unordered liver volume (ULV) / standard liver volume (SLV) and RILD was found: For patient Child-Pugh A, the ratio was < 50%; for Child-Pugh B patients, the rate is <30%
3. Both photon and PBT can achieve high local control rates with acceptable toxicity.
However, PBT has a better potential to deliver higher doses while maximizing the volume of undissected liver. Clinically, the reduction in normal liver dose achieved by PBT is not a serious requirement for all patients, as some patients may benefit from a smaller target volume of irradiation when available. may meet normal hepatic limitations. The 2018 Miami Liver Proton Therapy Conference reached consensus that patients who should be strongly prioritized for PBT include those with: At least Child-Pugh B cirrhosis, tumor-to-liver ratio high (ie, larger or smaller tumor size unresolved liver volume), a large number of tumors, or pre-hepatic radiation therapy. Dose comparison of proton therapy versus SBRT versus conventional radiotherapy for liver tumors is illustrated in Figure 1.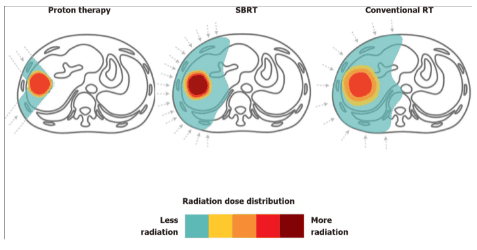
4. Role of radiotherapy in very early and early stage hepatocellular carcinoma
Early and very early hepatocellular carcinomas include those with BCLC classification 0-A, as follows: Carcinoma in situ; one tumor ≤ 2 cm, one tumor ≤ 5 cm, or three tumors <3 cm; and placed tumor burden in the Milan criteria, with Eastern Cooperative Oncology Group (PS) (PS) performance status 0 as well as Child-Pugh AB classification. For these HCC patients, although the standard of care remains surgery and RFA, SBRT is definitively a potential third-line treatment for medically inoperable, non-operating RFA conditions. treatable and difficult to treat; More notably, it can act as a bridge to liver transplantation5. Role of radiotherapy in intermediate-stage HCC
Intermediate-stage HCC includes individuals with BCLC class B, as follows: Multiple tumors, a single tumor > 5 cm, good patient status (eg, PS 0-1), as well as reserve good liver (eg, Child-Pugh AB). The tumor burden can be further subdivided, as follows: (1) In addition to the Milan criterion but within the Up to 7 criterion; and (2) Tumors exceeding Maximum 7 criteria. For these patients, only a limited number of cases can be treated with surgery or RFA. Several combined modality approaches, including local therapy, regional therapy, and systemic therapy, have been reported in association with CFRT and SBRT6. Role of radiotherapy in advanced HCC
Advanced-stage HCC included patients with BCLC class C, with criteria for portal vein invasion, vena cava/cardiac invasion or thrombosis, lymph node metastasis, and distant metastasis. and Child-Pugh AB. SBRT or conventional radiation therapy may be used in combination with other topical, topical, and systemic therapies to serve as a potentially curative or palliative treatment7. Role of radiotherapy in end stage HCC
End-stage HCC includes those with BCLC D classification, with Child-Pugh C or ECOG PS 3-4 criteria. For these patients, carefully planned SBRT is a safe bridge to liver transplantation in selected patients with a Child-Pugh score ≥ 8. Alternatively, SBRT or conventional radiation therapy may be used. to treat symptoms.
Conclusion
Currently, there are two motivations to improve the effectiveness of radiotherapy in HCC. One is technological advancement, which allows for precise delivery of SBRT, increased tumor control, and reduced adverse effects on surrounding normal tissues. The second is the explosion in the development of targeted therapies and checkpoint blockade immunotherapies, which prolong survival of HCC patients and re-emphasize the importance of tumor control at place. Currently, the role of radiation therapy in the treatment of HCC is being actively studied in combination with systemic therapies to induce the STAR effect.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.