This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine, Vinmec Central Park International General Hospital
Boerhaave's syndrome is caused by a ruptured esophagus caused by excessive vomiting. The disorder may present with vague symptoms or the classic Mackler triad of vomiting, chest pain, and subcutaneous emphysema (pneumothorax). Boerhaave syndrome is one of the most fatal gastrointestinal disorders, with a mortality rate of up to 40%.
1. History taking and clinical examination
Boerhaave Syndrome symptoms include vomiting, lower chest pain, and subcutaneous emphysema. Clinicians should suspect Boerhaave syndrome when a patient presents with chest pain with or without subcutaneous emphysema due to heavy drinking and vomiting. Up to a third of patients do not have these symptoms. The actual clinical presentation of Boerhaave syndrome will depend on the extent of the perforation, the extent of the leak, and the time since the onset of the lesion.
Usually, the patient will present with pain at the puncture site, usually in the neck, chest, epigastrium or upper abdomen. Perforation in the neck may be accompanied by neck pain, difficulty swallowing, or difficulty swallowing; perforation in the chest accompanied by chest pain; and intra-abdominal perforation accompanied by epigastric pain radiating to the shoulder or back. A history of increased pressure in the esophagus for any reason associated with chest pain should warrant immediate consideration of this condition. Physical examination findings may include vitreous abnormalities (tachycardia, tachypnea, fever), decreased breath sounds on the cloudy side, mediastinal emphysema, and Hamman's sign (mediastinal "explosive crackles"). accompanying each heartbeat) in the left concave position.
2. Subclinical
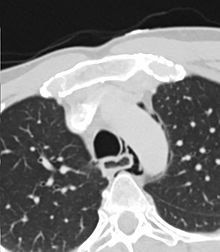
Unfortunately, laboratory tests are of little value in making a diagnosis; however, they can rule out the more common conditions in the difference including myocardial infarction and pancreatitis. Imaging is of high importance in the diagnosis of Boerhaave Syndrome. While a chest x-ray is available, it is normal in about 15% of cases and cannot be used to rule out the diagnosis. Possible chest X-ray findings include subcutaneous or mediastinal emphysema, mediastinal enlargement, pleural effusion, and in 20% of cases, the “V sign” (divided air streak). cut the cardiac planes behind the heart).
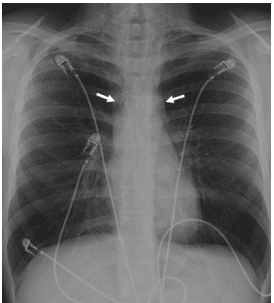
Hình 1: Hình ảnh X quang thể hiện tràn khí trung thất do hội chứng Boerhaave
Treatment is usually tailored according to the patient's presentation, type and extent of rupture, time of diagnosis, and viability of the esophageal wall. Early perforations, diagnosed within 12-24 hours, have the best outcome. Three common treatment options include conservative, endoscopic, or surgical. Primary treatment includes replacement of lost fluid, coverage of broad-spectrum antibiotics, and surgical evaluation. Surgical intervention includes repair of esophageal perforation through thoracotomy or diagnostic thoracoscopic surgery. Endoscopic stenting has been used to prevent fistula formation or to seal esophageal fistulas in both patients with late diagnosis and those with early diagnosis without extensive infection. Conservative treatment is usually reserved for small perforations. Controversy arises when a late perforation, those diagnosed after 24 hours, is diagnosed, because wound edges are often edematous, hard, or friable making repair risky. Taking this into consideration, many physicians treat late perforations through disruption of the pleural space and mediastinum, esophageal opening, and feeding gastrostomy. Esophageal reconstruction is usually done after 6 weeks. Nutritional supplementation is required if fasting is prolonged.
3. Differential diagnosis
Aortic dissection Acute pancreatitis Myocardial infarction Pneumothorax
4. Prognosis
Prognosis depends on the time of diagnosis. Delayed diagnosis and treatment often lead to poor outcomes. Those who are diagnosed and operated within 24 hours have a good prognosis with a survival rate of 75%.

Bệnh nhân được phẫu thuật trong 24h đầu thường có tiên lượng tốt hơn
5. Complications
Mediastinitis Massive pleural effusion Pneumomediastinum Empyema Subcutaneous emphysema Progressive respiratory distress syndrome Death Matters needing attention:
The diagnosis of Boerhaave syndrome requires a high degree of suspicion.
Delay in diagnosis can be fatal by several days.
Imaging should be completed with water-soluble contrast to avoid mediastinal contamination with barium contrast.
If the perforation is small, a watch-and-wait approach can be used but early surgery is recommended.
Diagnostic thoracoscopy is the gold standard of treatment.
6. Conclusion
The management of Boerhaave syndrome is a collaboration between specialties. Patients need immediate hydration, antibiotics, and surgical advice. Treatment is usually tailored according to the patient's presentation, type and extent of rupture, time of diagnosis, and viability of the esophageal wall. Early perforations, diagnosed within 12-24 hours, have the best outcome. Three common treatment options include conservative, endoscopic, or surgical. Primary treatments include volume replacement, broad-spectrum antibiotic coverage, and surgical evaluation. Surgical intervention includes major esophageal repair through thoracotomy or diagnostic and interventional thoracoscopy, which is the gold standard within the first 24 hours. Endoscopic stenting has been used to prevent fistula formation or seal esophageal fistula in both patients with late diagnosis and those with early diagnosis without extensive infection.
Conservative treatment is usually reserved for small perforations. Lately diagnosed patients often have multiple organ failure and death. Patients who receive early treatment usually have a good prognosis, but recovery can take several months.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Anisha R. Turner; Sherry D. Turner., Boerhaave Syndrome, StatPearls [Internet]. March 2, 2020. Prosperi P, Alemanno G, Di Bella A, Ardu M, Maltinti G, Iacopini V, Bergamini C, Valeri A. A minimally invasive approach with a 3d imaging system for the treatment of esophageal perforation due to Boerhaave syndrome. Ann Ital Chir. 2018 Dec 19;7 [PubMed] Cuccì M, Caputo F, Fraternali Orcioni G, Roncallo A, Ventura F. Transition of a Mallory-Weiss syndrome to a Boerhaave syndrome confirmed by anamnestic, necroscopic, and autopsy data: A case report. Medicine (Baltimore). 2018 Dec;97(49):e13191. [PMC free article] [PubMed] He F, Dai M, Zhou J, He J, Ye B. Endoscopic repair of spontaneous esophageal rupture during gastroscopy: A CARE compliant case report. Medicine (Baltimore). 2018 Nov;97(48):e13422. [PMC free article] [PubMed] Ciriano Hernández P, Grao Torrente I, Viejo Martínez E, Turégano Fuentes F. Boerhaave syndrome presenting as gastric emphysema. Cir Esp. 2019 Apr;97(4):231. [PubMed]