This is an automatically translated article.
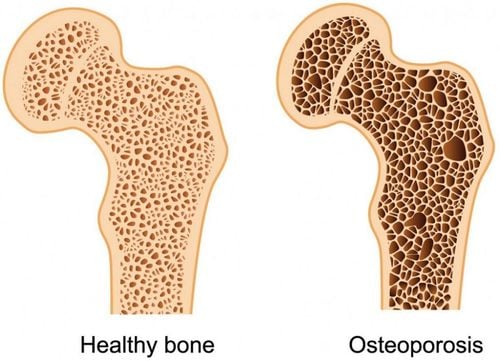
The word “osteoporosis” means “porous bone”. This is a disease that weakens bones, and if you have it, you're more at risk for a sudden and unwanted fracture. Osteoporosis means you lose bone and have less bone mass and strength. Currently, there are many drugs that increase bone formation to prevent bone loss or treat osteoporosis. So, what are the notes when using bone-building drugs? Let's read the article below to understand more.
An estimated 200 million people have osteoporosis around the world. Although osteoporosis occurs in both men and women, women are four times more likely to develop the disease than men. After age 50, one in two women and one in four men will experience an osteoporosis-related fracture in their lifetime. Another 30% have low bone density putting them at risk for osteoporosis. This condition is called osteoporosis.
Osteoporosis is the cause of more than two million fractures each year and this number is continuing to grow. There are steps you can take to prevent osteoporosis from occurring. Treatments can also slow the rate of bone loss if you have osteoporosis.
1. What is the treatment for osteoporosis?
Between the time you are young and your 30s, your body usually makes more bone than it loses. After the age of 35, bone breakdown occurs faster than bone accumulation, leading to a gradual loss of bone mass. If you have osteoporosis, you will lose bone mass at a greater rate. After menopause, the rate of bone breakdown is even faster.
As we age, the remodeling process can become unbalanced. More old bone is removed than new bone is created. Over time, this causes bones to weaken and break more easily. Many conditions can cause imbalanced bone regeneration including hormonal changes, certain medications, prolonged inactivity as well as other illnesses.
Bone can also be reabsorbed to replace essential minerals that are lacking in the blood. This happens when there is not enough calcium in the diet. The result of these processes is the same: Bone weakens slowly but steadily, which can eventually lead to osteoporosis and fractures.
The goal of osteoporosis therapy is to try to restore the balance of resorption and formation. It can be done by slowing resorption through the use of anti-deformation drugs or by promoting bone formation using anabolic drugs.
2. Medicines to treat osteoporosis or drugs to increase bone formation
All of these drugs reduce the chances of a fragile bone breaking. They come in many varieties, from daily tablets to annual intravenous infusions. There is no single drug that is best for everyone.2.1. Alendronate Sodium or Alendronate Sodium plus Vitamin D3 (Fosamax®, Fosamax Plus D and Binosto TM)
Alendronate is approved for the prevention and treatment of osteoporosis in postmenopausal women and for the treatment of osteoporosis in men. It is also approved to treat glucocorticoid-induced osteoporosis in men and women caused by long-term use of steroid medicines (eg, prednisone and cortisone). Alendronate reduces bone loss, increases bone density and reduces the risk of vertebral and hip fractures.
As a precaution, alendronate is taken daily as a 5 mg tablet or weekly as a 35 mg tablet. For treatment, it is taken daily as a 10 mg tablet, weekly as a 70mg tablet (with or without vitamin D3) or weekly as a 70mg effervescent tablet. The weekly dose with vitamin D3 contains 2,800 IU or 5,600 IU of vitamin D3.
The alendronate tablet must be taken first thing in the morning after waking up and on an empty stomach. It is recommended to take the tablet whole with about 200ml of water, at least 30 minutes before eating or drinking anything. Binosto effervescent tablets must be dissolved in 120ml of filtered water. The patient must remain upright (sitting, standing, or walking) during this 30-minute period. This careful dosing is necessary to ensure that alendronate is absorbed and to minimize the risk of esophageal irritation.
Alendronate with 2,800 IU or 5,600 IU vitamin D3 is another option for vitamin D. Weekly alendronate with 2,800 IU vitamin D3 is equivalent to taking 400 IU daily, while weekly alendronate with 5,600 IU vitamin D3 is the equivalent of taking 800 IU per day. Vitamin D3 is also known as cholecalciferol.
Alendronate được giúp phòng ngừa và điều trị loãng xương ở phụ nữ sau mãn kinh và điều trị loãng xương ở nam giới.
2.2. Ibandronate Sodium (Boniva®)
Ibandronate is approved for the prevention and treatment of osteoporosis in postmenopausal women. Ibandronate reduces the incidence of vertebral fractures. For both prevention and treatment, ibandronate is taken once a month as a 150mg tablet. For treatment, it is also available as an intravenous (IV) injection of 3mg every three months.
Oral ibandronate should be taken on the same day each month, in the morning upon waking and on an empty stomach. It is recommended to take the tablet whole with about 200ml of water, at least 60 minutes before eating or drinking anything. The patient must remain upright (sitting, standing or walking) during this 60-minute period. For adequate absorption of ibandronate and to minimize the risk of esophageal irritation.
The fourth dose will be prescribed by the doctor. Patients should have a blood test (serum creatinine) to confirm that kidney function remains normal before each IV injection.
2.3. Sodium Risedronate (Actonel®, Atelvia)
Risedronate (Actonel) is approved for the prevention and treatment of osteoporosis in postmenopausal women and for the treatment of osteoporosis in men. It is also approved for the prevention and treatment of glucocorticoid-induced osteoporosis in men and women caused by long-term use of steroid drugs (eg, prednisone and cortisone).Risedronate slows bone loss, increases bone density and reduces the risk of vertebral and non-fracture fractures, including hip fractures.
For prevention and treatment, risedronate is taken daily as a 5 mg tablet, weekly as a 35mg tablet available with or without a separate calcium carbonate tablet, or monthly as a 150mg tablet.
Actonel tablets should be taken first thing in the morning after waking up and on an empty stomach. It is recommended to take the tablet whole with about 200ml of water, at least 30 minutes before eating or drinking anything. Atelvia should be taken immediately after breakfast with at least 120ml of filtered water. Patients must remain upright (sitting, standing or walking) for at least 30 minutes after taking Actonel or Atelvia to allow adequate absorption and minimize the risk of esophageal irritation.
2.4. Zoledronic Acid (Reclast®)
Zoledronic acid is approved for the prevention and treatment of osteoporosis in postmenopausal women. It is also approved to increase bone mass in men with osteoporosis and to prevent new clinical fractures in patients with recent minor trauma hip fractures. In 2009, it was approved for the prevention and treatment of glucocorticoid-induced osteoporosis in men and women caused by long-term use of steroid drugs (eg, prednisone and cortisone).
Zoledronic acid is given once a year or every two years as an intravenous (IV) infusion to treat osteoporosis. Zoledronic acid increases bone density and reduces the incidence of vertebral and hip fractures.
The doctor will prescribe zoledronic acid injection as an intravenous (IV) dose of 5mg at a medical facility. Patients should have blood tests to check for creatinine and creatinine clearance before each IV dose to ensure that kidney function remains normal.
2.5. Denosumab (Prolia)
Denosumab is FDA-approved for the treatment of osteoporosis in postmenopausal women at high fracture risk and for increased bone mass in men with osteoporosis at high fracture risk. The drug is also approved to increase bone mass in men undergoing antiandrogen therapy for prostate cancer who are at high risk of fracture and to increase bone mass in women at risk. High fractures with aromatase inhibitor therapy for breast cancer. The U.S. Food and Drug Administration (FDA) has approved the use of Prolia® (denosumab) for the treatment of glucocorticoid-induced osteoporosis (GIOP) in men and women at high risk of fracture. identified as having a history of osteoporosis-related fractures, having multiple risk factors, for those with fractures, or for patients who have failed or are intolerant to other available osteoporosis therapy. This approval was based on data from a Phase 3 study that showed that glucocorticoid-treated patients receiving Prolia had higher bone mineral density (BMD) than those receiving an active comparator. risedronate).Denosumab is a human monoclonal antibody/RANK ligand inhibitor. Denosumab increases bone density and reduces the incidence of non-vertebral fractures, including hip fractures. It is indicated for injection once every 6 months.
Side effects
Denosumab can lower blood calcium levels. If the blood calcium level was low before taking denosumab then the low calcium level must be corrected before giving the medicine or the disease will get worse. Patients should have a blood test after each dose to confirm that their blood calcium levels are not abnormally low. Signs of low calcium levels include spasms, convulsions or cramps in the muscles; numbness and tingling in your fingers, toes, or around your mouth. If any of the above symptoms are observed while taking this medicine, the patient should contact their doctor. However, most patients with low calcium levels do not have these signs.
People with weakened immune systems or taking other medicines that affect the immune system may have an increased risk of getting a serious infection with denosumab. Even patients without immune system problems have a higher risk of certain infections such as skin infections. Patients should contact their doctor immediately if there are signs of infection. These signs may include fever, chills, red and swollen skin, skin that is hot or painful to the touch, severe pain in the abdomen, pain or burning when urinating, or urinating more often and in small amounts. .
Denosumab can also cause a skin rash. Call your doctor right away if you notice any unusual skin-related symptoms. Any discomfort or pain in the groin or thigh should be reported to your doctor, as should any unhealed oral lesions. Patients should take good care of their teeth during treatment and should have their teeth examined by a doctor or dentist before starting medication.

Denosumab làm tăng mật độ xương và giảm tỷ lệ gãy xương sống, được chỉ định tiêm mỗi 6 tháng 1 lần.
2.6. Calcitonin-Salmon (Fortical® and Miacalcin®)
Calcitonin is a synthetic hormone for the treatment of osteoporosis in postmenopausal women who are at least 5 years postmenopausal when other medications have not been suitable. This hormone is involved in calcium regulation and bone metabolism.
Calcitonin slows down bone breakdown and increases bone density in the spine. It reduces the risk of spinal fractures but has not been shown to reduce the risk of non-vertebral or hip fractures. Calcitonin is available as a nasal spray (200 IU daily) or 100 IU daily as a subcutaneous or intramuscular injection.
Side Effects
Common side effects with calcitonin in the nose are runny nose, headache, back pain, and nosebleeds. Calcitonin injection can cause allergic reactions and unpleasant side effects including flushing of the face and hands, increased urination, nausea, and skin rashes.
Because there may be a link between cancer and the use of calcitonin, it is important to talk with your doctor regularly when taking this medicine.
2.7. Menopausal Hormone Therapy (MHT)
Menopausal hormone therapy (MHT) is approved to prevent osteoporosis in postmenopausal women. MHT reduces bone loss, increases bone density in both the spine and hips, and reduces the risk of hip and spine fractures and other diseases in postmenopausal women. MHT also relieves menopausal symptoms.
MHT is usually available as a tablet or a skin patch (transdermal) and in other forms and in a variety of dosages.
Side effects
When using only estrogen, it can increase a woman's risk of developing cancer of the lining of the uterus (endometrial cancer). To reduce this risk, doctors prescribe the hormone progesterone in combination with estrogen (hormone therapy or HT) to women with a uterus. Estrogen therapy (ET) is indicated for women who have had a hysterectomy. Side effects may include vaginal bleeding in women with a uterus above the HT, breast tenderness, and gallbladder disease.
Research by the Women's Health Initiative (WHI) has confirmed that one type of HT, Prempro® (given to the average woman more than ten years after menopause), reduces the risk of hip fracture and other diseases, as well as colon cancer. However, it is associated with a slightly increased risk of breast cancer, stroke, heart attack, venous blood clots, and cognitive (mental) decline. Although ET was associated with similar increases in the risk of stroke, venous blood clots, and cognitive decline, it did not increase the risk of breast cancer or heart attacks.
Women who have an early menopause or whose ovaries are removed in their 30s or early 40s may benefit from low-dose MHT. The results of the WHI study do not apply to women in this age group. Women who have had breast cancer or are at high risk for breast cancer should not consider MHT.
According to the FDA, postmenopausal women should consider other osteoporosis medications before taking MHT to prevent osteoporosis. Because estrogen use has risks, women should discuss it with their doctor to see if the benefits outweigh the risks. Women who decide to take MHT should take the lowest possible dose for the shortest time to control menopausal symptoms and achieve their desired goals. When MHT is discontinued, bone loss can be rapid and other drugs should be considered to maintain the increase in bone density.
2.8. Raloxifene (Evista®)
Raloxifene is approved for the prevention and treatment of osteoporosis in postmenopausal women. It is in a class of drugs known as estrogen agonists/antagonists that have been developed to provide the beneficial effects of estrogen without all the potential downsides. It is not an estrogen, nor is it a hormone. Raloxifene is sometimes called a selective estrogen receptor modulator (SERM).Raloxifene reduces the risk of spinal fractures. There are no data to show that raloxifene reduces the risk of hip fractures and other non-spine conditions. For prevention and treatment, raloxifene is taken daily as a 60mg tablet, with or without meals.
Raloxifene seems to reduce the risk of estrogen-dependent breast cancer by 65% over 8 years. It is FDA approved to reduce the risk of invasive breast cancer in postmenopausal women with osteoporosis and even in women without osteoporosis at high risk for breast cancer. Raloxifene does not reduce the risk of coronary heart disease.
Side effects
Side effects include hot flashes, leg cramps and an increased risk of deep vein thrombosis (blood clots). Other side effects include swelling and temporary flu-like symptoms. Raloxifene is not associated with diseases of the uterus or ovaries and does not affect cognitive (psychiatric) function.
Women at risk of stroke should not take Raloxifene. This includes women who have had a previous stroke, transient ischemic attack (TIAs), atrial fibrillation (a type of severe irregular heartbeat), or uncontrolled hypertension (high blood pressure). ).
2.9. Tissue Selective Estrogen Complex: Conjugated Estrogen / Bazedoxifene (Duavee®)
The combination of conjugated estrogens and bazedoxifene is approved for women with moderate to severe hot flashes associated with menopause and also to prevent postmenopausal osteoporosis. The drug combines estrogen with bazedoxifene, an estrogen agonist/antagonist (also called SERM). In women 1 to 5 years after menopause, use of this combination increased spine bone mineral density on average at 12 months compared with those who did not take the drug. The hip bone mineral density also increased after 12 months compared with those who did not take the drug.
Each daily pill contains 0.45mg of conjugated estrogen and 20mg of bazedoxifene and can be taken with or without meals.
Conjugated estrogens/bazedoxifene should only be used by postmenopausal women who still have a uterus. The bazedoxifene in this medicine reduces the risk of overgrowth of the uterine lining that can occur with the estrogen component. Therefore, women taking this drug do not need to take a progestin.
When used to prevent menopausal osteoporosis, talk with your doctor about whether another treatment or medication without estrogen might be better for you. Also, you should take this medicine for the shortest possible time and only for the time it needs to be treated.
Side Effects
Because it contains estrogen, the same precautions and warnings for estrogen apply to conjugated/bazedoxifene estrogens. Women who cannot take estrogen or hormone therapy should not take conjugated estrogens/bazedoxifene. Side effects may include muscle spasms, nausea, pain, and dizziness.
2.10. Teriparatide Parathyroid hormone (PTH) (1-34) (Forteo®)
Teriparatide, a parathyroid hormone, is approved to treat osteoporosis in postmenopausal women and in men who are at high risk of fracture. It is also approved to treat osteoporosis in men and women who are at high risk of fractures from long-term steroid use. This drug rebuilds bone and significantly increases bone mineral density. Teriparatide reduces the risk of vertebral fractures and no fractures.
Teriparatide is self-administered as a daily subcutaneous injection from a prefilled pen containing a four-week supply. It can be done for up to two years. By the end of two years, bone loss can be rapid. To retain the benefits of teriparatide treatment, most experts recommend that patients begin anticoagulation immediately after teriparatide therapy is finished.
Side effects
Side effects may include leg cramps, nausea and dizziness. Lowest increases in serum and urinary calcium may occur, but no increased risk of kidney stones has been reported.
In animal studies performed in immature rats, very high doses of teriparatide used for long periods of time increased the incidence of osteosarcoma, a type of bone cancer. Although common in mice, this type of tumor is extremely rare in adults. According to experience with teriparatide in humans, to date, there is no evidence of an increased risk of osteosarcoma.
Who should not take this medicine:
People with Paget's disease of bones. Children have growing bones. People with unexplained elevated alkaline phosphatase (alkaline phosphatase is a specific blood test). People who have had radiation treatment involving the skeleton. It is not recommended for people with metabolic bone diseases such as hyperparathyroidism and people with cancer that has spread to the bones. People with certain abnormal blood tests, including elevated calcium levels, should also not take this medicine.
2.11. Romosozumab-aqqg (Evenity®)
Romosozumab-aqqg is approved for the treatment of osteoporosis in postmenopausal women at high risk for fracture defined as: History of osteoporosis fractures, multiple fracture risk factors, and patients who have had failure or intolerance to other available osteoporosis therapies.
Romosozumab-aqqg is a humanized monoclonal antibody (IgG2) produced in a mammalian cell line by recombinant DNA technology that binds and inhibits sclerostin.
Romosozumab-aqqg is given as two separate subcutaneous injections, administered one after the other for a total dose of 210mg. 12 doses should be injected once a month into the abdomen, thighs or upper arms.
The anabolic effect of Romosozumab-aqqg gradually decreased after 12 monthly therapeutic doses. Therefore, you should limit your use to 12 monthly doses. If osteoporosis therapy is warranted, you should consider continuing anti-spondylolisthesis therapy.

Romosozumab-aqqg được tiêm với hai mũi tiêm dưới da riêng biệt, tiêm lần lượt để tiêm tổng liều 210mg.
3. When should you take bone-building drugs?
Women whose bone density test results show a T-score of -2.5 or less, such as -3.3 or -3.8, should begin treatment to reduce fracture risk. Many women need treatment if they are at risk for osteoporosis (a condition where bone weakness is not as severe as osteoporosis).
Your doctor can use the World Health Organization or FRAX fracture risk assessment tool to see if you qualify for treatment based on risk factors and density results your bone. People who have had a typical osteoporosis fracture, such as in the wrist, spine, or hip, should also be treated (sometimes even if bone density results are normal).
Supplements
It's important to remember supplements and diet. Also, even though a supplement is a tonic, that doesn't mean it's safe for everyone.
Your doctor will likely ask you to get enough calcium and vitamin D. This is important if you have osteoporosis or if you are trying to prevent it. Ideally, you can get these substances through your diet, but if you can't do that, supplements are a reasonable option. There are plant-based calcium supplements, some of which are derived from algae.
The recommended daily intake of calcium is 1,000mg to 1,200mg per day through diet and/or supplements. Taking more than this amount of calcium has not been shown to provide additional bone strength but may be associated with an increased risk of kidney stones, calcium buildup in blood vessels and constipation.
Opinions vary on how much vitamin D is needed but the truth is that many people don't get enough and need to take a supplement. Your doctor can check your blood levels and then make recommendations based on these results.
You and your doctor need to discuss the benefits of taking which medications or supplements are right for you and the benefits and side effects of taking it.
4. How long to take bone-building drugs?
Romosozumab-aqqg, Teriparatide, and Abalo Parade are the only osteoporosis drugs with a defined duration of treatment. The FDA recommends that treatment be limited to no more than 18 months or two years. There is a great deal of variation in the ideal duration of treatment for other drugs.
Some drugs, like raloxifene and denosumab, leave the body quickly. Their effects usually go away after a person stops taking them. Some drugs, like bisphosphonates, stay in your bones after you stop taking them - some longer (alendronate, zoledronic acid) than others (risedronate, ibandronate). They can continue to function and provide protection even after a person stops using them. The most effective regimen and duration depends on the individual drug, the individual patient, and their degree of fracture risk.
Like any medicine, osteoporosis drugs can only work if they are taken as prescribed. With many health conditions, it can be easy for you to remember to take your medicine because without it, you will feel bad. Your blood pressure goes up or some other obvious problem is the result. That doesn't happen with osteoporosis. Without a bone density test, you might not even know you have osteoporosis until you break a bone. Similarly, when you take medicine for osteoporosis, you may not feel like your bones are getting stronger. You can only be sure that you have reduced your risk of osteoporosis fractures.
It is important that you take your medicine and take it consistently. If you have any trouble following your treatment plan, or if you are concerned about side effects, talk to your doctor. They will help you find the medication that works best for you. There are many different options out there, one of which is sure to suit your needs.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference articles: nof.org, webmd.com, clevelandclinic.org